Objective: Reconstruction of extensive chest wall defects following bilateral mastectomy presents significant challenges, particularly when the defect spans from the clavicle to the xiphisternum. This report describes the use of a bipedicled deep inferior epigastric perforator flap to address such complex defects while preserving donor-site function and minimizing morbidity through an integrated reconstructive strategy.
Case Presentation: A 51-year-old woman with bilateral invasive ductal carcinoma presented with an ulcerative lesion on the right breast and a palpable mass in the left. Imaging revealed large, multicentric tumors with bilateral axillary lymphadenopathy. Following suboptimal response to neoadjuvant chemotherapy, she underwent radical mastectomy on the right, including en bloc resection of the pectoralis major muscle, and modified radical mastectomy on the left. This resulted in a massive right-sided chest wall defect measuring 45 × 17 cm, and a smaller contralateral defect requiring bilateral reconstruction.
Management and Outcome: Preoperative computed tomographic angiography identified four robust medial row perforators. A bipedicled deep inferior epigastric perforator flap measuring 42 × 16 cm was harvested, with bilateral internal mammary arteries selected as recipient vessels to enable tension-free anastomoses and symmetric perfusion. Abdominal wall integrity was preserved through muscle-sparing dissection, limited undermining, and submuscular mesh reinforcement. The patient recovered uneventfully and was discharged on postoperative day five. At six-month follow-up, clinical assessment and BREAST-Q scores demonstrated complete wound healing, preserved abdominal strength, and high satisfaction across all domains.
Conclusion: This case illustrates the feasibility and clinical value of an integrated reconstructive approach incorporating bipedicled deep inferior epigastric perforator flap transfer, bilateral internal mammary artery anastomoses, and abdominal wall reinforcement. The strategy achieved durable coverage, maintained donor-site function, and optimized both functional and aesthetic outcomes in the setting of massive chest wall reconstruction following bilateral mastectomy.
Reconstruction of extensive chest wall defects following radical mastectomy remains a formidable surgical challenge. This is especially true in cases involving large, full-thickness defects. Conventional reconstructive options, such as the latissimus dorsi (LD) flap, the transverse rectus abdominis myocutaneous (TRAM) flap, and the thoracoepigastric flap, have demonstrated clinical utility in various scenarios. However, defects extending from the clavicle to the xiphisternum often exceed the coverage capacity and vascular reliability of these techniques. In such cases, alternative strategies are required to provide sufficient soft tissue volume, stable perfusion, and acceptable functional and aesthetic outcomes [1,2].
Bipedicled DIEP Flap as an Alternative
To meet this reconstructive demand, the bipedicled deep inferior epigastric perforator (DIEP) flap has emerged as a promising option for anterior chest wall resurfacing. This technique offers extensive soft tissue coverage while preserving abdominal wall musculature and minimizing morbidity at the donor site [3]. It was initially developed for breast reconstruction in patients with either midline abdominal scars or high-volume tissue requirements. The bipedicled DIEP flap recruits bilateral abdominal tissue and maintains perfusion through two independent deep inferior epigastric pedicles, which enhances both reliability and reach [4]. In patients undergoing bilateral mastectomy for locally advanced breast cancer, where both resection and structural loss are substantial, this approach offers a practical solution to achieve long-lasting wound coverage without compromising donor-site integrity.
Viability Concerns and Knowledge Gaps
Despite its advantages, bilateral DIEP flap use introduces significant concerns regarding abdominal wall viability. This is particularly relevant when both deep inferior epigastric arteries and internal mammary arteries (IMAs) are sacrificed [5,6]. Vascular compromise in this context may increase the risk of postoperative complications such as hernia or bulging. To minimize these risks, careful preoperative planning is essential, including assessment of perfusion territories and strategies for abdominal wall reinforcement. Published literature remains limited on the specific outcomes and technical challenges of using bipedicled DIEP flaps in large, non-breast chest wall defects. This gap underscores the importance of further case-based evaluations and detailed surgical analyses.
Aim of the Present Report
To address this knowledge gap, we present a case involving successful reconstruction of a massive right chest wall defect using a bipedicled DIEP flap following bilateral mastectomy. This report outlines the surgical rationale, vessel selection, flap design, and donor-site management strategies implemented to achieve reliable coverage while minimizing complications. Through this technical description, the case aims to contribute to ongoing advancements in autologous reconstruction for complex thoracic defects.
A 51-year-old woman presented with a three-month history of an ulcerative lesion on the right breast. She reported no significant family history of breast carcinoma and tested negative for BRCA1 and BRCA2 mutations. Clinical examination revealed an ulceroproliferative mass with overlying skin erosion on the right breast. A distinct, firm mass was palpable in the left breast. Bilateral axillary lymphadenopathy was also evident.
Histopathological evaluation of biopsy specimens from both breasts confirmed invasive ductal carcinoma. The tumor in the right breast had a Ki-67 proliferation index of 10%, was positive for estrogen receptor (ER) and progesterone receptor (PR), and exhibited human epidermal growth factor receptor 2 (HER2/neu) expression scored as 2+ by immunohistochemistry with negative results on fluorescence in situ hybridization (FISH). The tumor in the left breast was grade 2, showed a Ki-67 index of 18%, and was also ER and PR positive. HER2/neu expression in the left lesion was similarly equivocal (2+) by immunohistochemistry and FISH negative.
Staging with positron emission tomography–computed tomography (PET–CT) revealed large, multicentric tumors in both breasts. The lesion in the right breast measured 4.5 cm and demonstrated invasion of the pectoralis major muscle. A presternal subcutaneous nodule and right axillary lymph node involvement were also observed. Bilateral tumors were classified as T3, N2, with no evidence of distant metastasis. These findings corresponded to a clinical stage of cT3N2M0.
The patient received neoadjuvant chemotherapy consisting of four cycles of doxorubicin (Adriamycin) and cyclophosphamide (AC regimen), followed by four cycles of docetaxel. Owing to a suboptimal clinical response, she subsequently underwent extensive surgical resection.
Surgical Procedure
Bilateral mastectomy and chest wall resection
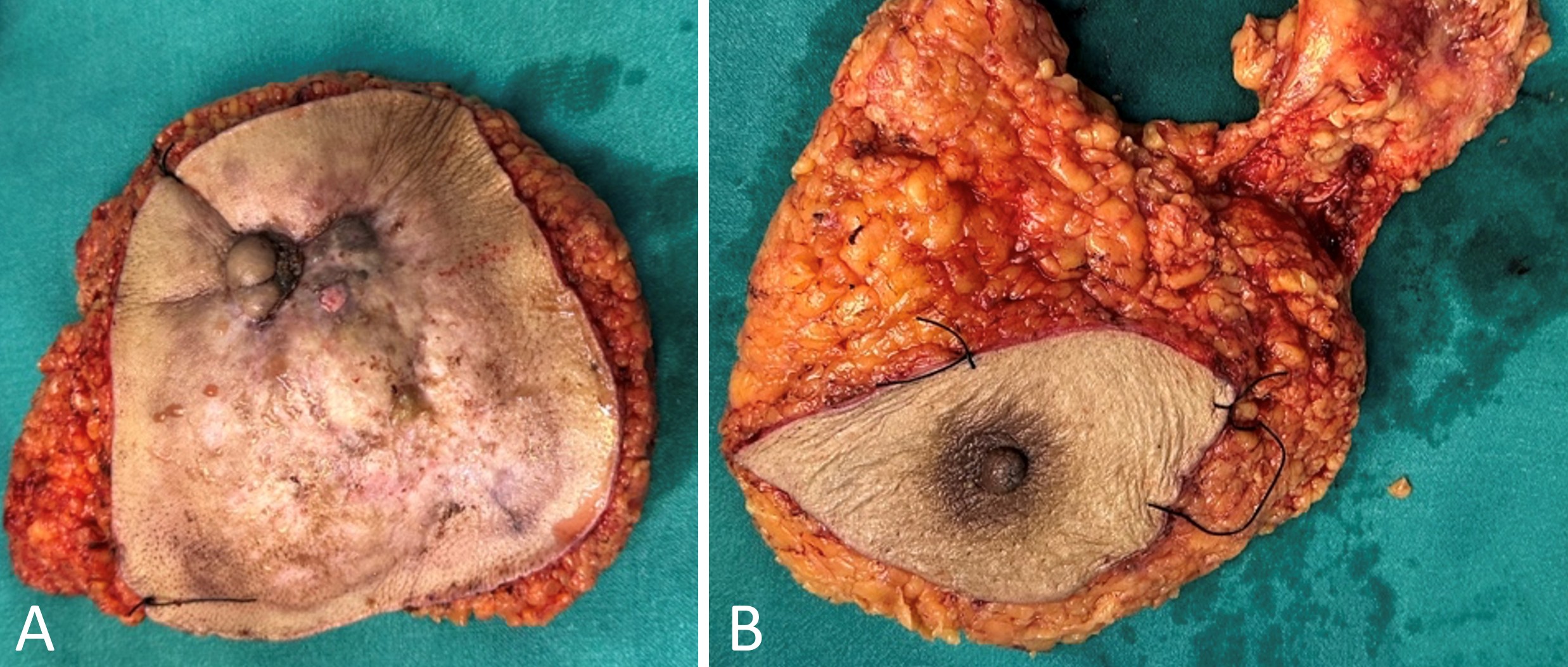
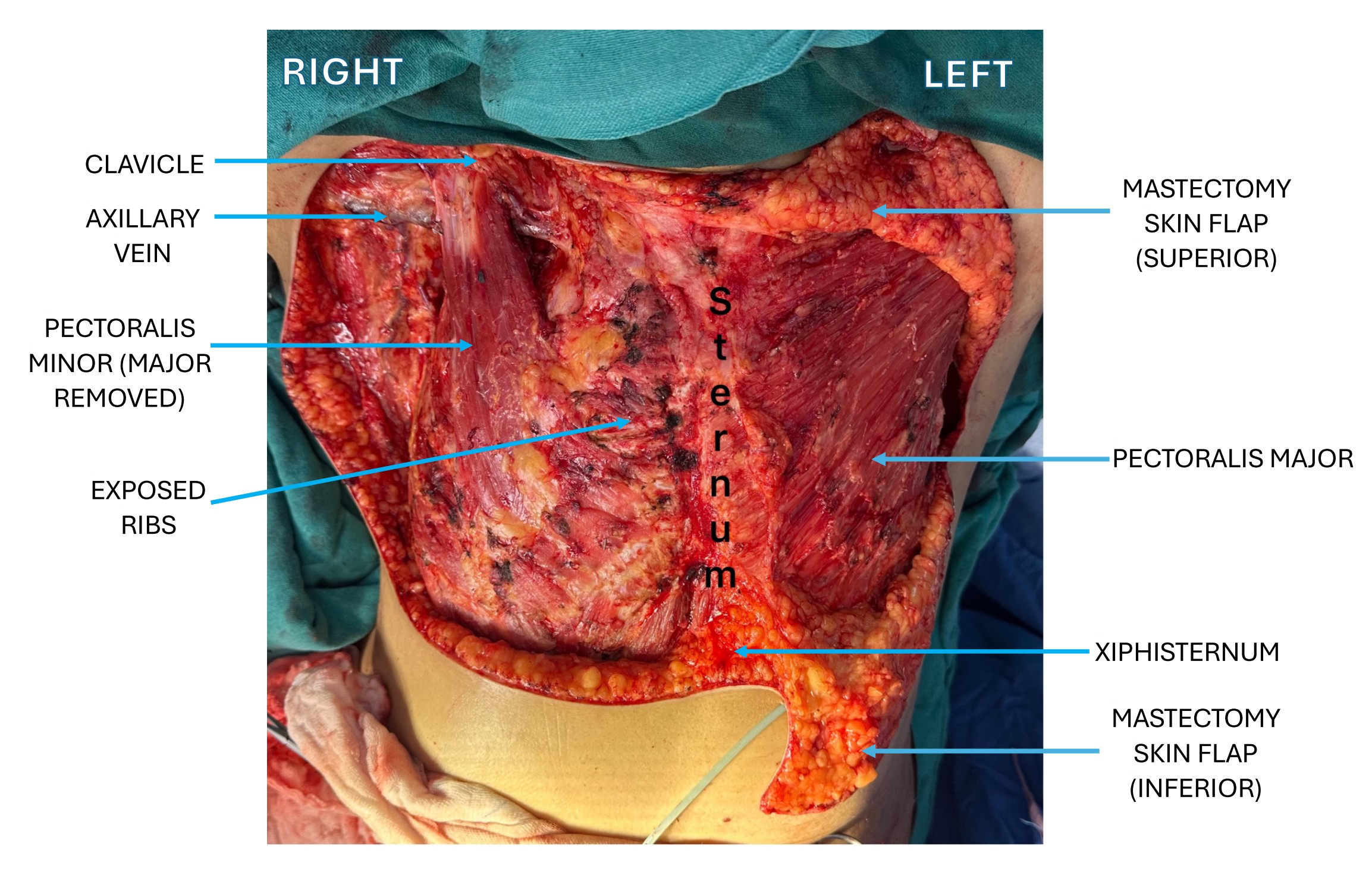
We performed a right-sided radical mastectomy with en bloc resection of the entire breast tissue. This included removal of the nipple–areolar complex, the pectoralis major muscle, and the axillary lymph nodes (Figure 1A). We preserved the pectoralis minor muscle. This procedure resulted in a substantial chest wall defect measuring 45 cm × 17 cm. The defect extended from the midline of the sternum to the lateral chest wall, reaching superiorly to the clavicle and inferiorly to the xiphisternum (Figure 2).
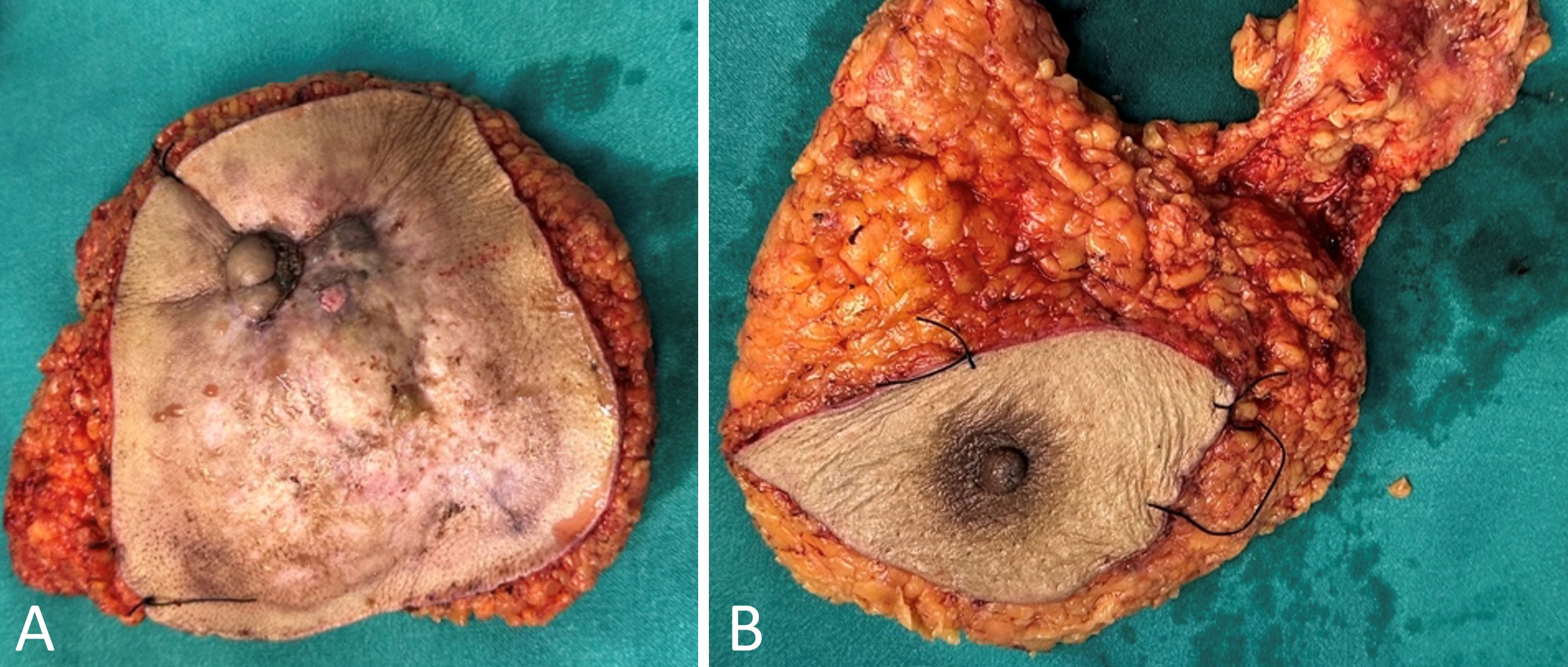
Figure 1. Right and left resection specimens. (A) Specimen from the right breast following radical mastectomy, showing an ulceroproliferative growth with involvement of the nipple–areolar complex. The resected tissue includes pectoralis major muscle, axillary lymph nodes, and surrounding adipose tissue. (B) Specimen from the left breast following modified radical mastectomy. The nipple–areolar complex is centrally located. The pectoralis major muscle is preserved. The specimen includes breast tissue, axillary lymph nodes, and adipose tissue. Resection margins are marked with sutures.
On the left side, we performed a modified radical mastectomy involving en bloc excision of the entire breast tissue along with axillary lymphadenectomy (Figure 1B). We preserved the pectoralis major muscle, in accordance with standard technique to minimize chest wall morbidity while ensuring oncologic adequacy. Although the left-sided defect was smaller than the right, it still required careful surgical planning to enable effective reconstruction (Figure 2).
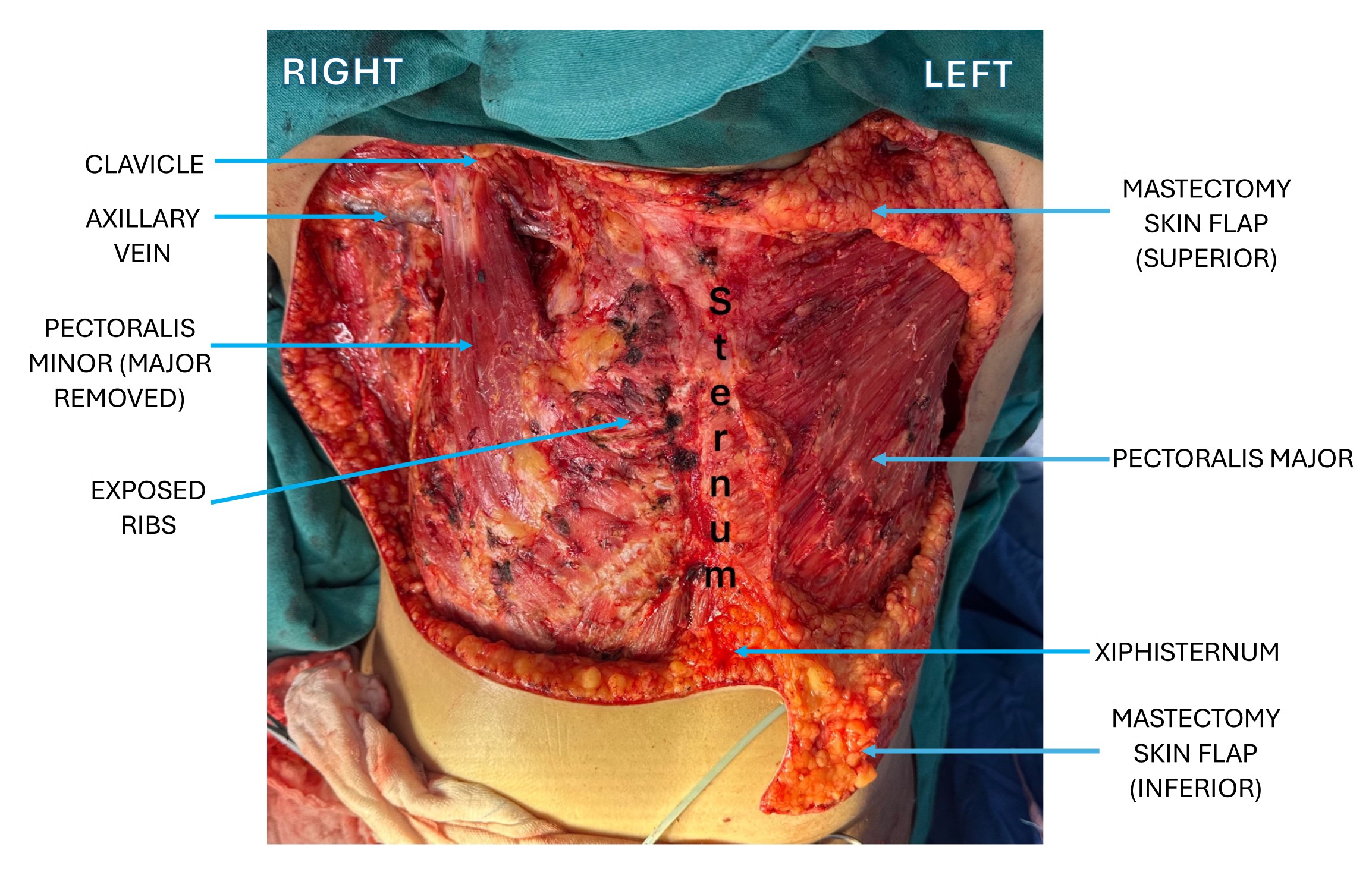
Figure 2. Bilateral chest wall defects after mastectomy. Intraoperative photograph showing an extensive right-sided defect after radical mastectomy, with tissue loss extending from the clavicle to the xiphisternum and crossing the midline. The defect exposes the underlying ribs and intercostal muscles. The pectoralis major muscle is removed, and the pectoralis minor muscle is preserved. The left side shows a smaller, well-defined defect after modified radical mastectomy, with the pectoralis major muscle preserved.
Preoperative planning and vascular mapping
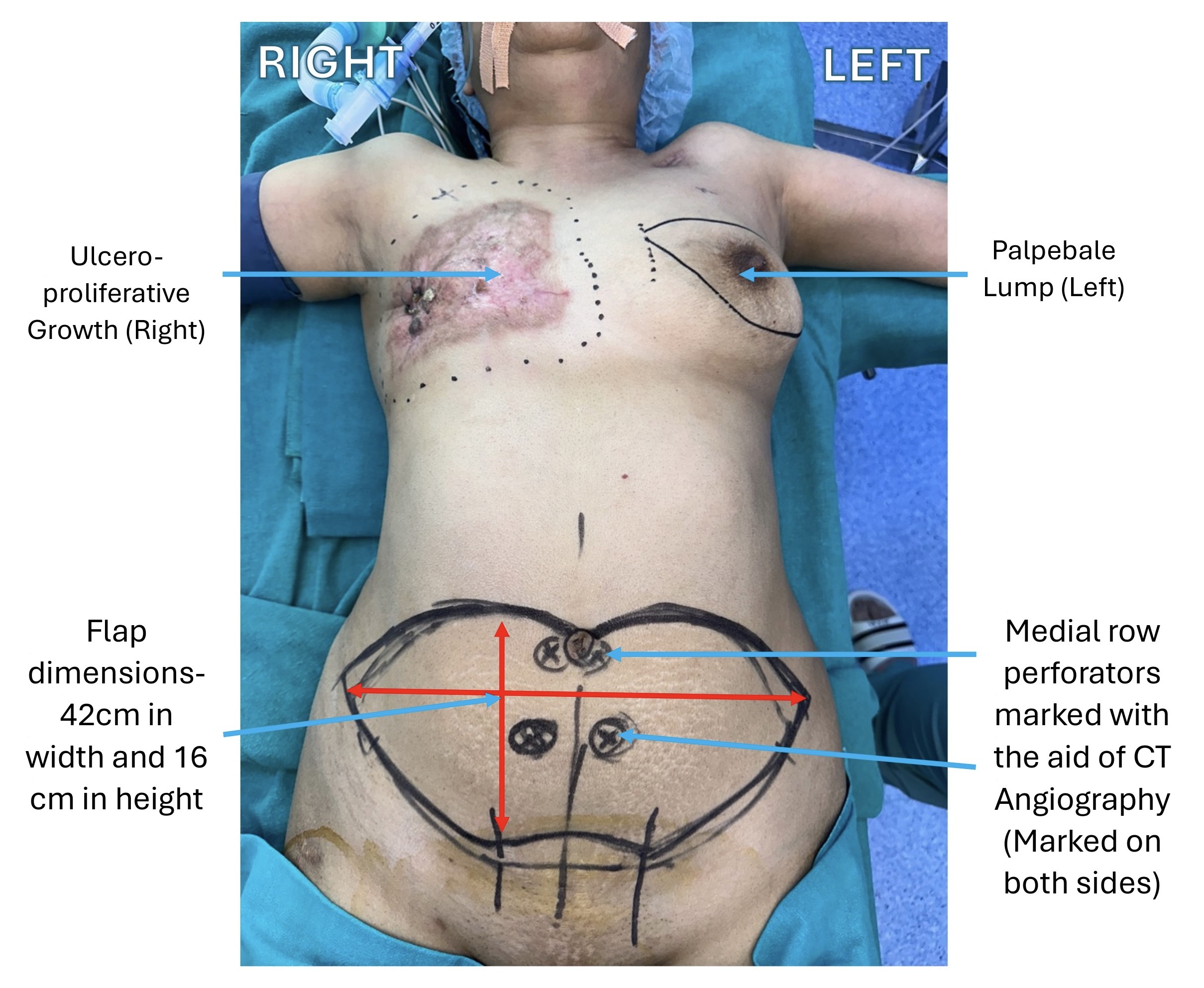
We began the bipedicled DIEP flap procedure with comprehensive preoperative planning. We used CT angiography to map the vascular anatomy of the abdominal wall and to identify bilateral medial and lateral row perforators (Figure 3). These perforators were essential to ensure consistent and reliable perfusion throughout the entire flap.
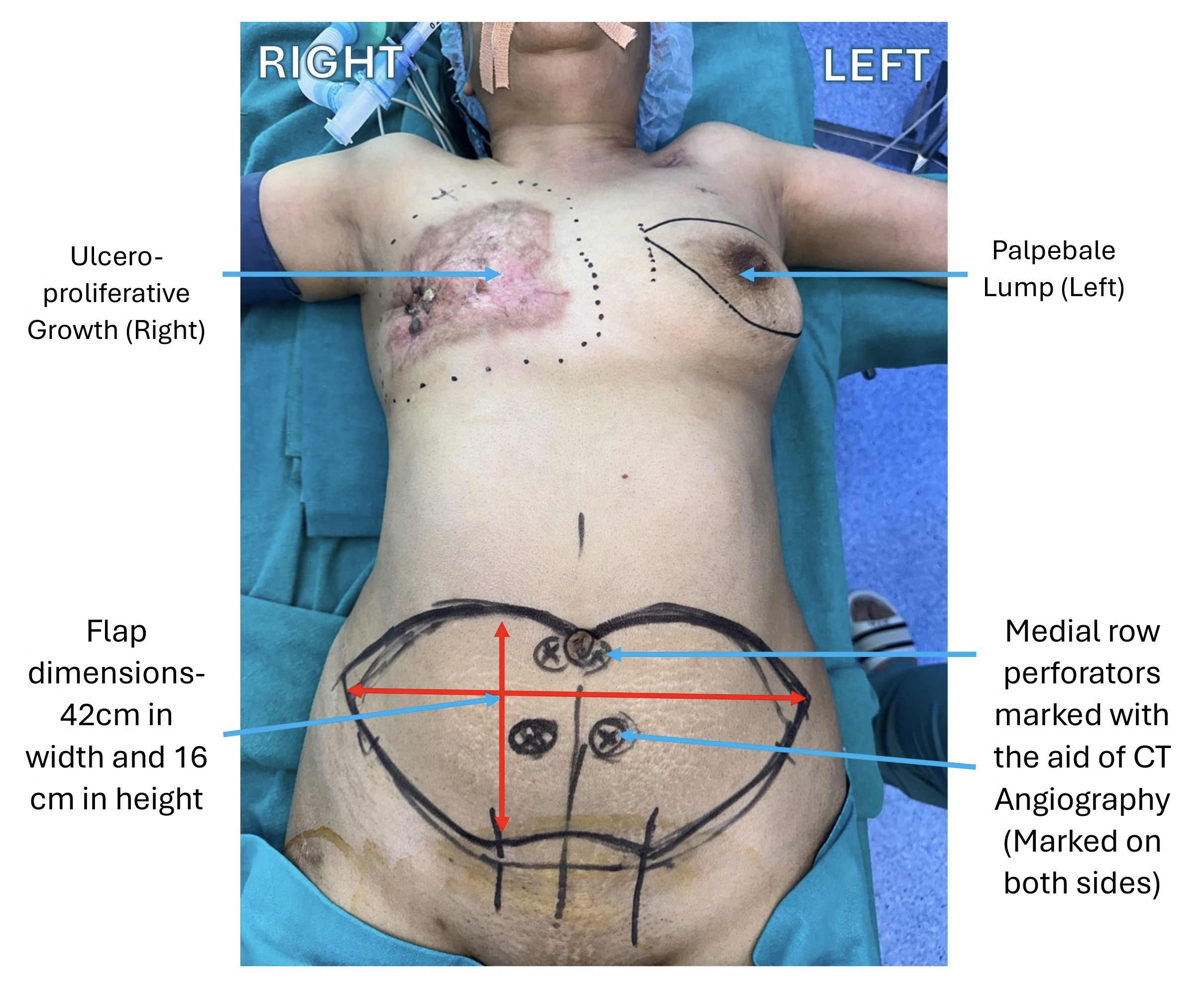
Figure 3. Preoperative markings for bilateral mastectomy and abdominal flap design. An ulceroproliferative lesion is visible on the right chest, and a palpable breast lump is outlined on the left. The lower abdomen is marked for harvest of a bipedicled deep inferior epigastric perforator flap. Bilateral medial row perforators, identified using computed tomography angiography, are indicated to ensure adequate vascular supply. The planned flap measures 42 cm in width and 16 cm in height. These markings guide flap design, perforator dissection, and chest wall reconstruction.
Perforator selection and flap design
We selected four dominant medial row perforators, including two from each side of the abdomen. Selection was based on vessel diameter and the course of each vessel through the muscle. We designed the flap to cross the abdominal midline, which maximized its reach and allowed optimal orientation for chest wall coverage. To guide flap design and ensure adequate tissue volume, we used key anatomical landmarks such as the umbilicus, midline, costal margin, and iliac crest. We marked the abdomen accordingly for flap harvesting, as shown in Figure 3.
Flap elevation and muscle preservation
We initiated flap elevation from the lateral aspect and advanced medially. During the dissection, we preserved the perforators with precision and minimized disruption to the rectus abdominis muscle. We identified bilateral medial row perforators arising from the deep inferior epigastric arteries. We then carefully dissected each perforator to preserve vascularity to both the medial and lateral portions of the flap. We harvested a flap composed of skin and subcutaneous tissue, measuring 42 cm × 16 cm, while fully preserving the rectus muscle.
Minimizing donor-site morbidity
We limited abdominal undermining to the minimum extent necessary to reduce the risk of donor-site complications. This approach preserved perfusion to the remaining abdominal wall and minimized the risk of devascularization. We harvested both deep inferior epigastric arteries in continuity with the flap and maintained the entire construct as a single, uninterrupted unit across the midline.
Bilateral IMA Strategy
We performed bilateral microvascular anastomoses to the internal mammary vessels using an end-to-end configuration. Arterial anastomoses were completed by hand suturing. For the venous connections, we used a coupler device. We selected the IMAs as recipient vessels because of their consistent caliber and robust flow characteristics. These features are essential to ensure reliable perfusion across the entire surface area of the bipedicled flap. By utilizing both IMAs, we achieved optimal flap orientation. This allowed complete and tension-free coverage of the chest wall defect. In addition, this strategy preserved the LD muscle as a backup reconstructive option in the event of flap compromise.
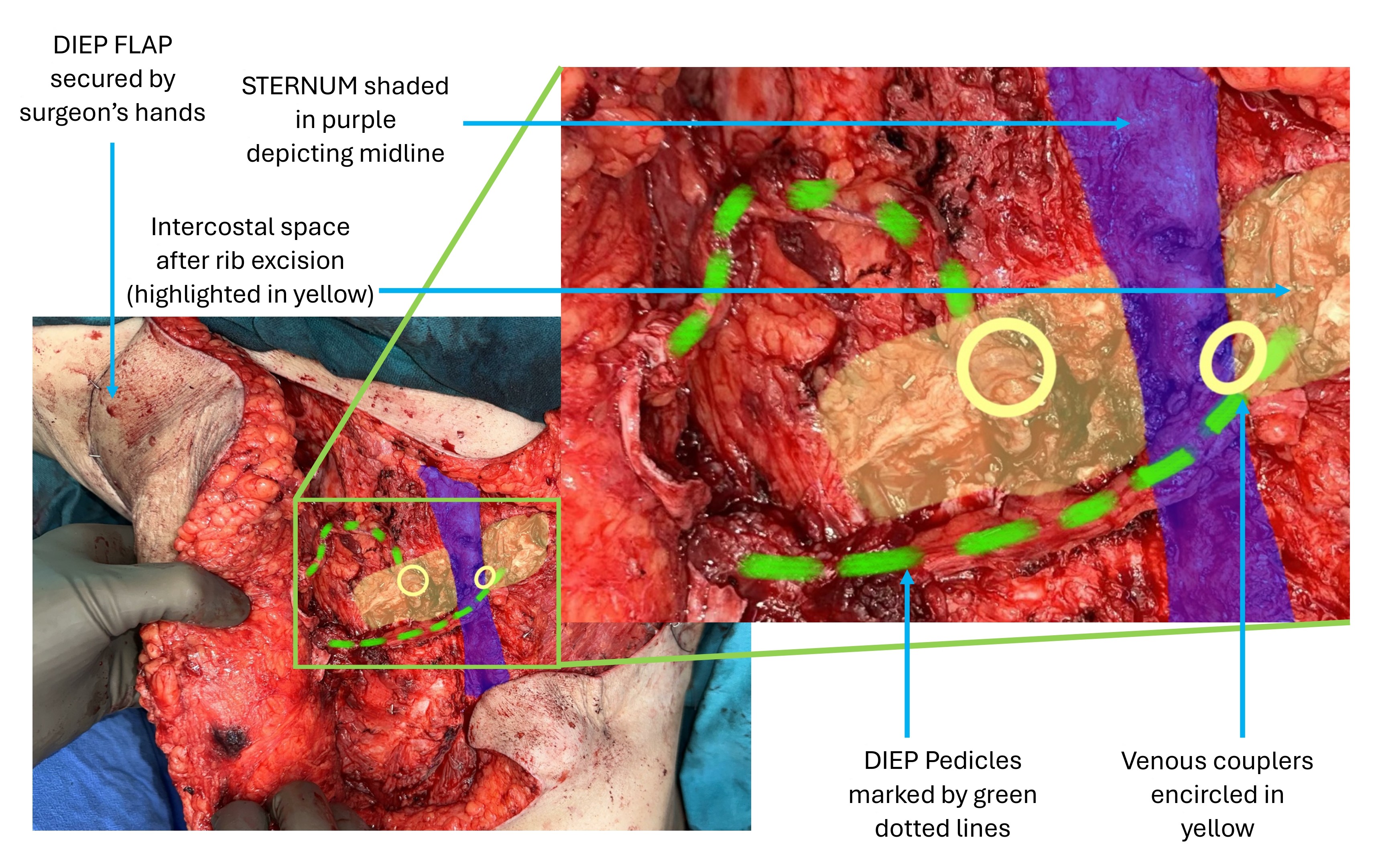
Flap orientation and pedicle alignment
We inset the flap at an oblique angle to facilitate tension-free alignment of the vascular pedicles. This orientation optimized the anastomotic geometry and minimized the risk of kinking or compression. Figure 4 illustrates the spatial relationship of the pedicles relative to the midline.
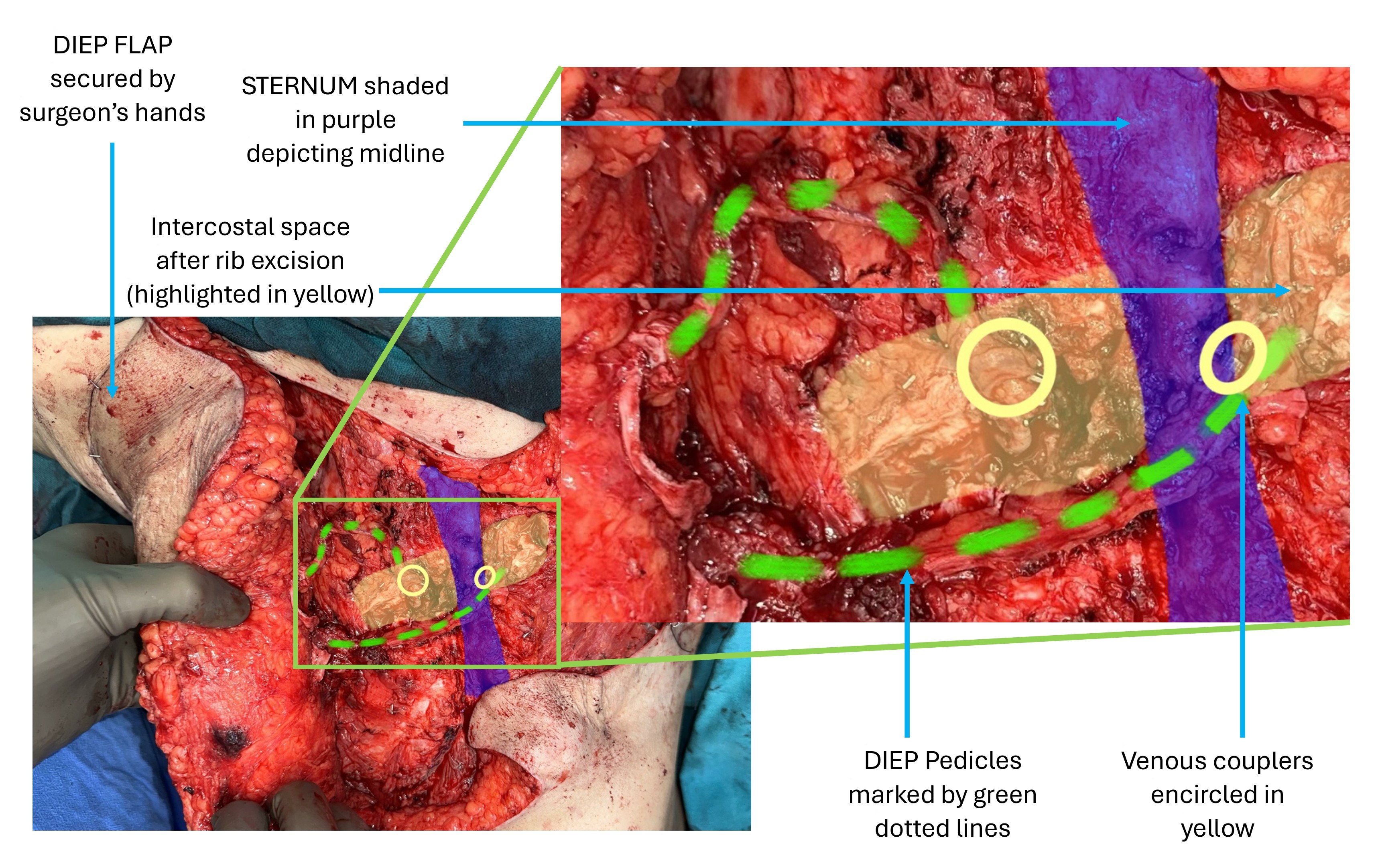
Figure 4. Intraoperative view of pedicle orientation and recipient site exposure, The deep inferior epigastric perforator flap is secured in position across the chest. The sternum, shaded in purple, marks the midline. Intercostal spaces exposed after rib resection are highlighted in yellow. Vascular pedicles are traced by green dotted lines. Venous couplers, marked by yellow circles, correspond to the sites of venous anastomosis.
Abdominal wall closure
We closed the rectus sheath primarily with 1-0 Stratafix suture material. To reinforce the abdominal wall, we positioned a Prolene mesh in the submuscular plane. We intentionally avoided supraumbilical undermining to preserve pannus vascularity and reduce the risk of devascularization.
Surgical Outcome
Early postoperative recovery
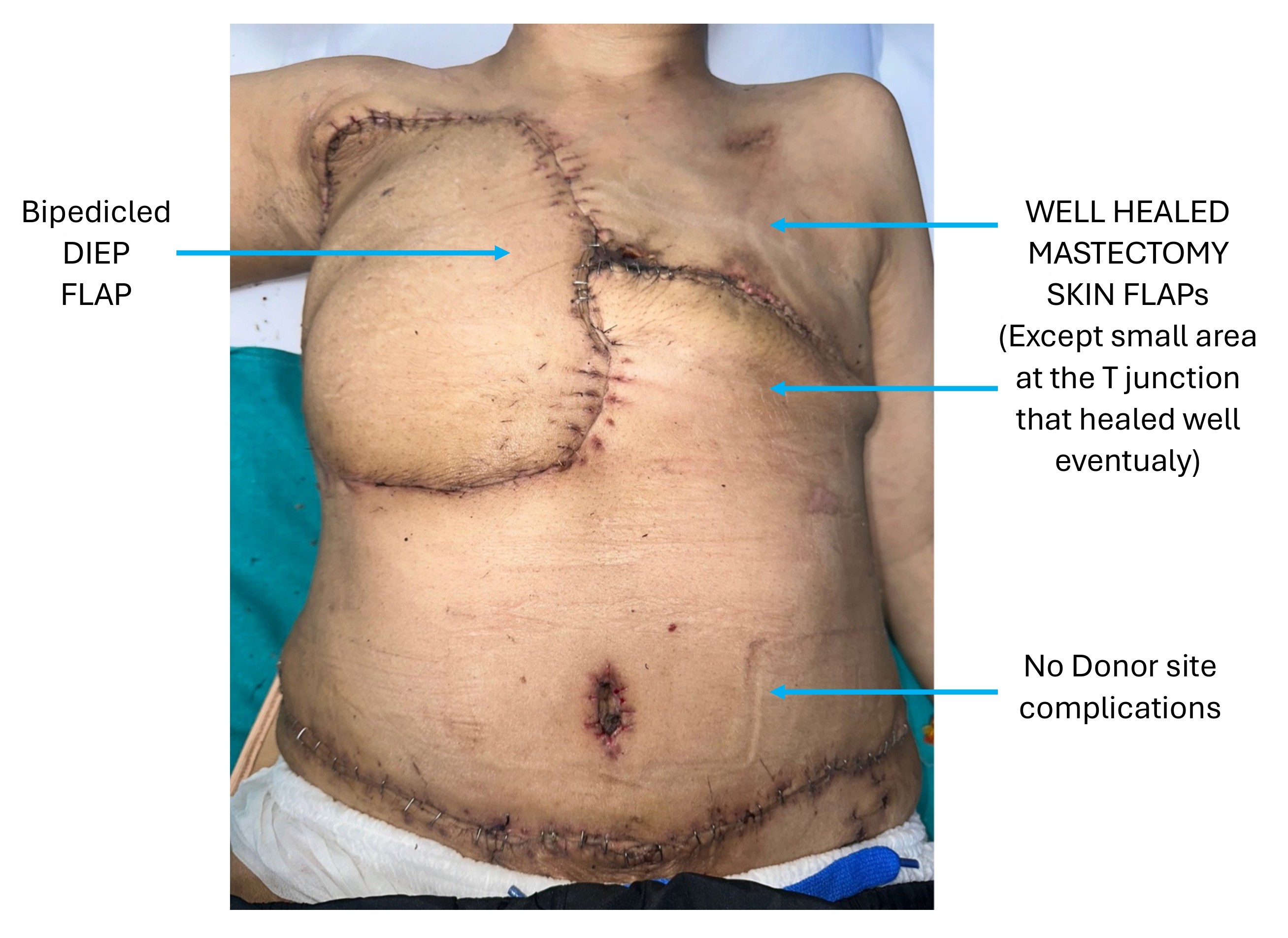
The patient recovered without complications and was discharged on the fifth postoperative day. At the two-week follow-up, the flap remained stable, and the mastectomy skin flaps appeared viable without signs of ischemia or necrosis (Figure 5). A minor area of delayed healing was noted at the T-junction but resolved spontaneously without the need for intervention. The abdominal donor site showed complete wound closure, with no evidence of dehiscence or other complications.
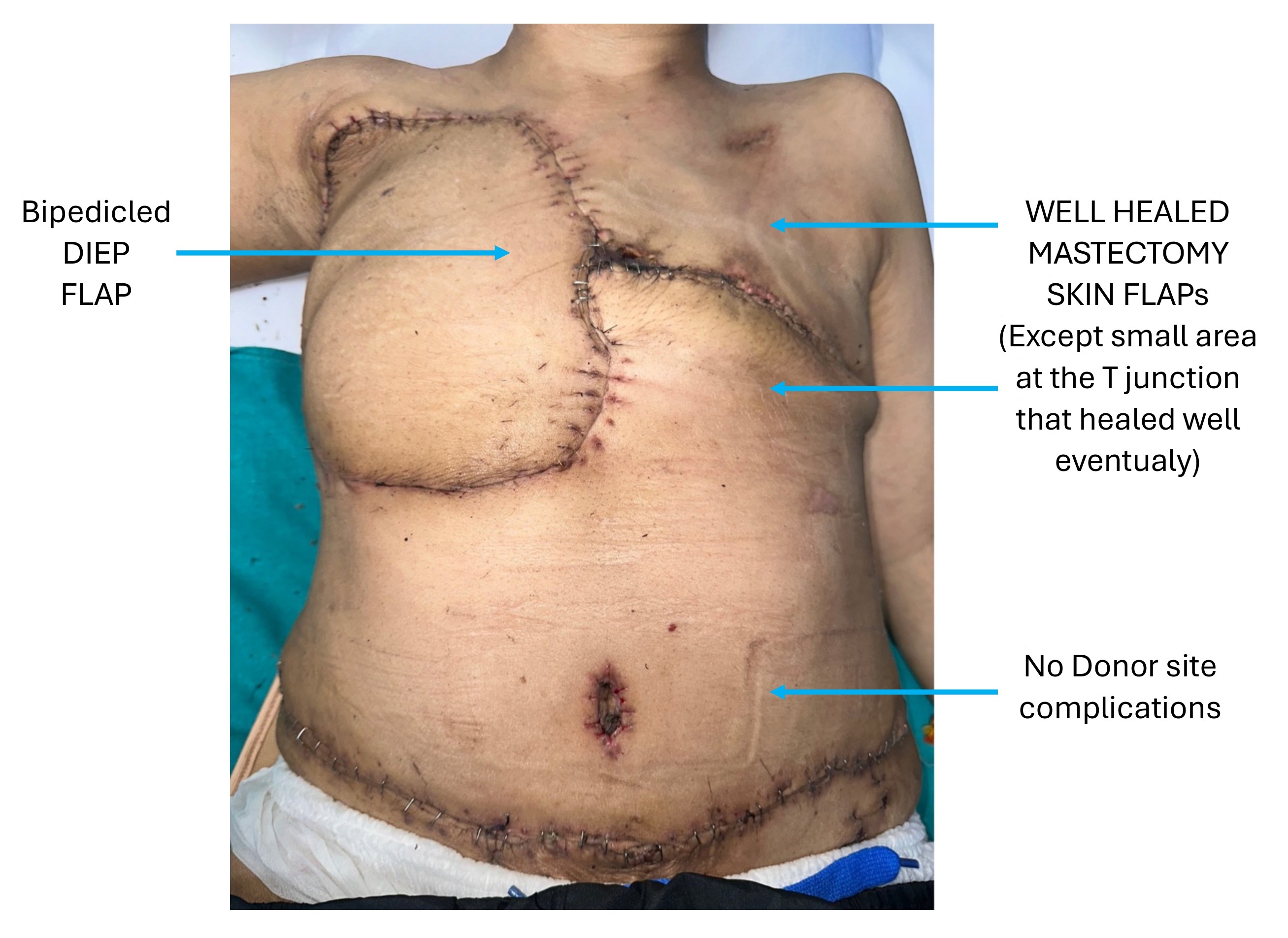
Figure 5. Postoperative appearance two weeks after bipedicled deep inferior epigastric perforator flap reconstruction. The anterior torso shows stable flap inset and well-healed mastectomy skin flaps. A small area of delayed healing is noted at the T-junction but resolved without intervention. The abdominal donor site demonstrates complete closure without dehiscence or other complications.
Six-month functional assessment
At the six-month follow-up, comprehensive clinical evaluation and patient-reported outcomes indicated favorable functional recovery. Assessment was conducted using the BREAST-Q questionnaire, a validated tool that quantifies patient satisfaction and quality of life following breast surgery across multiple domains [7]. Scores range from 0 to 100, with higher values reflecting more favorable outcomes. In this case, the patient reported high levels of satisfaction, with a breast satisfaction score of 78, a psychosocial well-being score of 85, and a physical well-being score of 82.
Donor-site and flap integrity
No clinical evidence of flap necrosis, donor-site hernia, or abdominal wall weakness was observed. Physical examination confirmed preservation of abdominal wall function, with no signs of structural compromise. Abdominal muscle strength was maintained, and no functional deficits were identified throughout the follow-up period.
Overall surgical efficacy
The reconstructive outcome demonstrated sustained flap viability, complete wound healing, and preserved donor-site integrity without evidence of ischemia, necrosis, or hernia formation. Functional recovery was favorable, as reflected by high BREAST-Q scores across aesthetic, psychosocial, and physical domains. Abdominal wall strength remained intact, and no functional impairments were identified during follow-up. Collectively, these findings support the reliability and clinical applicability of the bipedicled DIEP flap in managing extensive chest wall defects while minimizing donor-site morbidity.
This case presents a 51-year-old female with bilateral invasive ductal carcinoma of the breast and large anterior chest wall defects following bilateral mastectomy, with the right side being more extensive. A bipedicled DIEP flap was used for reconstruction, allowing tension-free anastomoses to bilateral IMAs while preserving abdominal wall integrity. The patient achieved favorable recovery, with high BREAST-Q scores and no complications at six months. This case highlights the clinical utility of the bipedicled DIEP flap in managing extensive bilateral defects and underscores its value as a muscle-sparing option in complex chest wall reconstruction.
Abdominal Wall Perfusion Strategy
Ensuring adequate abdominal wall perfusion is a critical consideration in bipedicled DIEP flap reconstruction, particularly when bilateral IMAs are utilized as recipient vessels. In this case, preoperative assessment with CT angiography and the abdominal wall pinch test confirmed sufficient perfusion across the donor site. To preserve native vascular integrity, lateral segmental blood supply was maintained, and undermining was limited to only what was essential. These intraoperative strategies minimized the risk of ischemia. Additional perfusion from the lateral intercostal and subcostal arteries contributed reliable collateral flow, supporting the viability of the remaining abdominal wall and contributing to a favorable reconstructive outcome.
Recipient Vessel Rationale
Bilateral IMAs were selected as recipient vessels to provide robust and symmetrical vascular inflow to the bipedicled flap. Their anatomical trajectory allowed tension-free pedicle alignment and optimal flap orientation, while preserving the LD muscle as a contingency option in the event of flap compromise. The IMAs were further favored due to their consistent caliber, reliable positioning, and technical ease of microvascular anastomosis. Although alternative recipient vessels such as the thoracodorsal and lateral thoracic arteries were evaluated, they were ultimately excluded because their anatomical orientation and limited reach were not well suited to the geometric requirements of a large bipedicled flap.
Technical Considerations and Procedural Complexity
The bipedicled DIEP flap is inherently more complex than either the LD or unilateral DIEP flap due to the requirement for bilateral microvascular anastomoses and meticulous bilateral perforator dissection. This increased technical demand typically extends operative time by one to two hours. However, prolonged operative duration does not necessarily lead to extended hospitalization. Enhanced recovery protocols have enabled similar lengths of stay across flap types, generally ranging from four to six days [8]. In this case, the patient recovered uneventfully and was discharged on postoperative day five.
The additional surgical time reflects the complexity of bilateral IMA anastomosis and the precision required to achieve balanced and reliable flap perfusion. High-level microsurgical expertise is essential to prevent complications such as venous congestion and to ensure vascular integrity across the entire flap. As such, successful execution of this procedure hinges on rigorous preoperative planning and advanced surgical proficiency.
Patient Selection Criteria and Risk Considerations
Ideal candidates for bipedicled DIEP flap reconstruction include patients with massive chest wall defects following radical mastectomy, those requiring large-volume autologous breast reconstruction, and individuals with midline-spanning defects that cannot be adequately addressed using a unilateral flap. This approach is also appropriate in cases of locoregional recurrence requiring complex reconstruction, provided that bilateral perforator anatomy is favorable and confirmed on preoperative CT angiography [3].
CT angiography serves a critical role in mapping the number, caliber, and anatomical course of perforators, with particular attention to the identification of bilateral medial row vessels to ensure symmetrical and reliable flap perfusion. Strong, well-positioned perforators should be prioritized to obviate the need for fallback options such as muscle-sparing TRAM or conventional TRAM flaps, which are associated with increased donor-site morbidity and abdominal wall dysfunction.
Additional risk factors must be carefully evaluated during patient selection. Elevated body mass index (BMI >30), poorly controlled diabetes, and underlying cardiac comorbidities are all associated with increased rates of fat necrosis, delayed wound healing, and perioperative complications [9]. A particularly critical consideration is the long-term impact of harvesting bilateral IMAs on future cardiac interventions. In patients with known or suspected coronary artery disease, the use of IMAs may preclude their availability for coronary artery bypass grafting. Therefore, preoperative assessment must weigh the reconstructive benefits of enhanced flap perfusion against the potential compromise of future cardiac surgical options [10].
Comparison with Muscle-Based and Alternative Flaps
Compared with conventional muscle-based and regional flaps, the bipedicled DIEP flap offers several advantages in the reconstruction of extensive chest wall defects. TRAM flaps, which involve harvest of the rectus abdominis muscle, are associated with elevated rates of abdominal wall complications such as hernia and bulging, with reported incidences ranging from 9% to 24% [11,12]. In contrast, DIEP flaps preserve the rectus muscle, substantially reducing donor-site morbidity while maintaining abdominal wall integrity. Hernia rates as low as 1.26% have been reported following DIEP reconstruction [13].
LD flaps remain a reliable option for moderate-sized chest wall defects due to their consistent vascularity and arc of rotation. However, they frequently require skin grafting to achieve complete coverage, and the limited tissue volume may compromise long-term durability and aesthetic outcomes. By comparison, the bipedicled DIEP flap provides a broader and well-perfused surface area, enabling single-stage reconstruction without the need for secondary grafting.
Thoracoepigastric flaps offer thin, pliable tissue with minimal donor-site morbidity but are constrained by limited flap size and arc of rotation. Omental flaps are highly vascularized and beneficial in irradiated or contaminated fields. However, they require intra-abdominal access and often necessitate skin grafting, thereby increasing operative complexity and recovery burden.
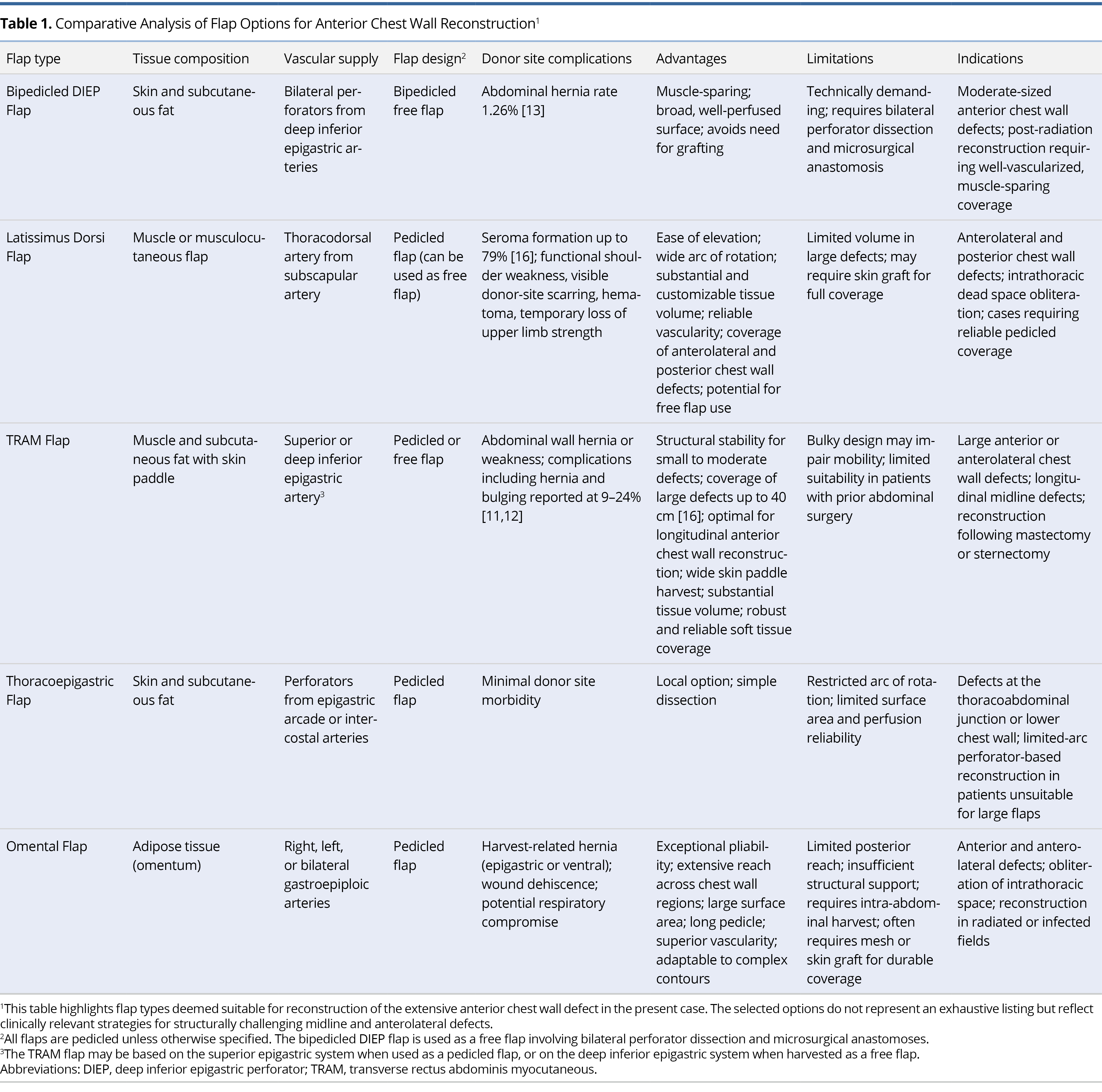
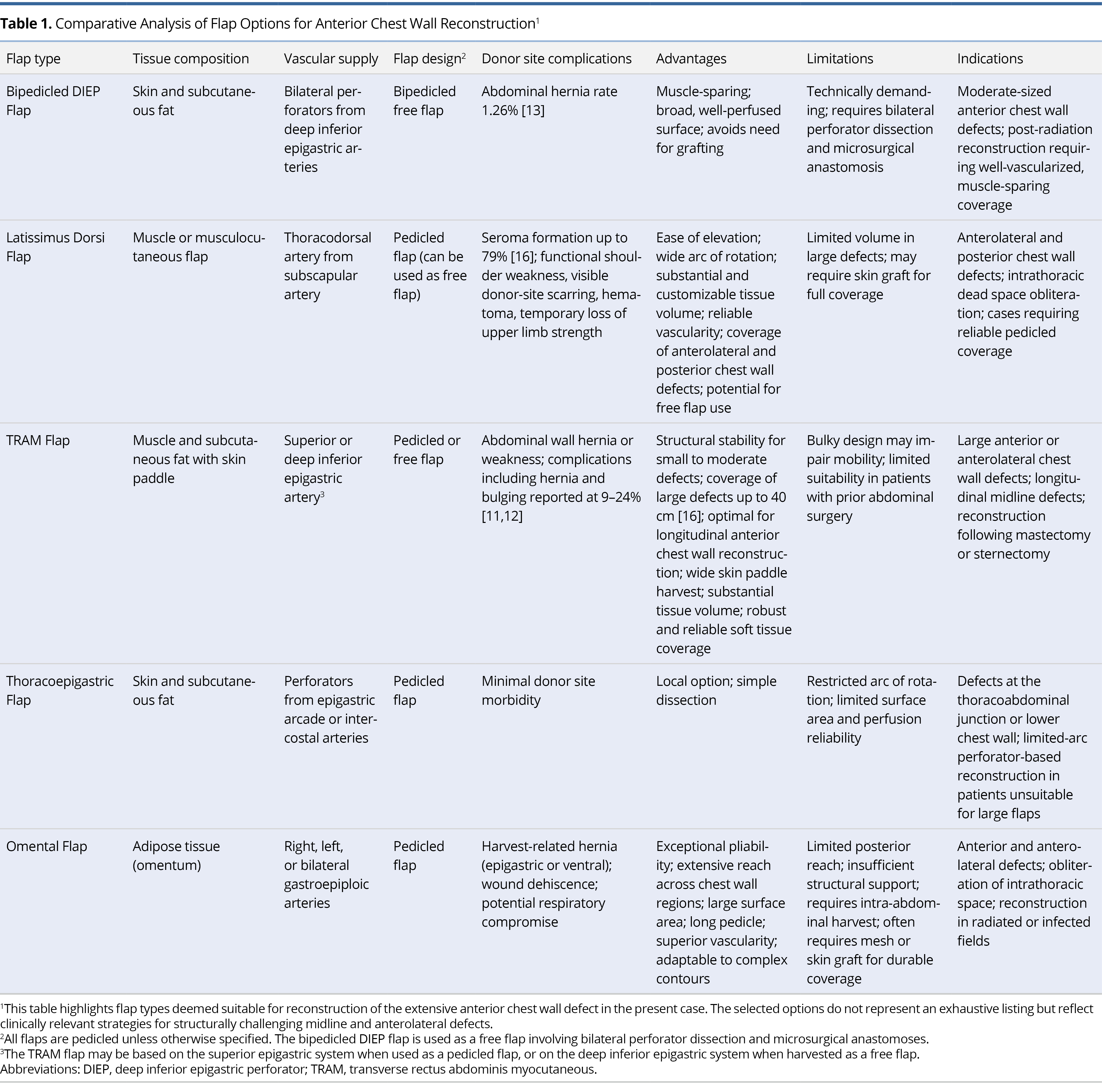
Overall, the bipedicled DIEP flap demonstrates several distinct advantages. It enables tension-free reconstruction of extensive chest wall defects, preserves functional musculature, minimizes donor-site morbidity, and eliminates the need for secondary grafting. Table 1 provides a structured comparison of flap options commonly used for reconstructing large or complex chest wall defects. It highlights key differences in anatomical composition, perfusion reliability, donor-site impact, and procedural complexity [11–17].
Postoperative Recovery and Functional Outcomes
Clinical follow-up at three and six months demonstrated favorable outcomes. Flap viability was maintained, abdominal wall function was preserved, and no postoperative complications were noted. At the six-month evaluation, BREAST-Q scores indicated excellent patient-reported outcomes, with scores of 78 for breast satisfaction, 85 for psychosocial well-being, and 82 for physical well-being. These results are consistent with prior studies showing that muscle-sparing techniques, such as the DIEP flap, are associated with reduced donor-site morbidity and improved outcomes in physical function, body image, and psychosocial health when compared to muscle-based reconstructions [5,12,18].
Objective assessments corroborated these subjective findings. Physical examination and abdominal wall strength testing revealed no evidence of flap necrosis, hernia, or muscular weakness. These observations support published data reporting lower donor-site complication rates with DIEP flaps relative to TRAM and LD flaps [17]. The preservation of abdominal wall integrity highlights a key advantage of the bipedicled DIEP approach. By sparing the rectus muscle, this technique facilitates early mobilization, enhances functional recovery, and minimizes long-term morbidity, particularly in reconstructions requiring both substantial volume and durable coverage [5,13].
Although CT imaging was not routinely employed in this case, it remains a useful adjunct for detecting subclinical donor-site abnormalities. Incorporating such imaging into postoperative follow-up protocols may improve the objectivity of functional assessments and enable earlier identification of potential complications.
Study Limitations
This report presents a single case, limiting the generalizability of its findings. Anatomical and oncologic differences among patients can significantly influence surgical outcomes, and results should therefore be interpreted with caution. Although the six-month follow-up provides initial clinical insights, it does not allow for evaluation of long-term complications, including donor-site hernia, bulging, or functional deterioration. Longer-term monitoring, with imaging and objective functional assessments, is needed. The bipedicled DIEP flap procedure also poses challenges in clinical implementation, as it demands advanced microsurgical skills and extended operative time, which may not be feasible in resource-limited settings. In addition, the lack of direct comparison with other reconstructive options prevents evaluation of its relative efficacy. Future studies should involve larger patient cohorts, extended follow-up, and controlled comparisons to establish the broader clinical utility of this technique.
This case illustrates the utility of the bipedicled DIEP flap in reconstructing extensive anterior chest wall defects after mastectomy. Bilateral IMAs ensured reliable, symmetrical perfusion, while the LD muscle was preserved as a backup option. Strategic planning, including limited abdominal undermining and targeted perforator selection, allowed tension-free inset and minimized donor-site morbidity. The reconstruction achieved durable coverage with preserved abdominal wall integrity, functional restoration, and favorable aesthetics. These findings support the bipedicled DIEP flap as a dependable and muscle-sparing option for large-volume chest wall reconstruction.
Received date: April 14, 2025
Accepted date: June 11, 2025
Published date: July 01, 2025
The manuscript has not been presented or discussed at any scientific meetings, conferences, or seminars related to the topic of the research.
The study adheres to the ethical principles outlined in the 1964 Helsinki Declaration and its subsequent revisions, or other equivalent ethical standards that may be applicable. These ethical standards govern the use of human subjects in research and ensure that the study is conducted in an ethical and responsible manner. The researchers have taken extensive care to ensure that the study complies with all ethical standards and guidelines to protect the well-being and privacy of the participants.
The author(s) of this research wish to declare that the study was conducted without the support of any specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The author(s) conducted the study solely with their own resources, without any external financial assistance. The lack of financial support from external sources does not in any way impact the integrity or quality of the research presented in this article. The author(s) have ensured that the study was conducted according to the highest ethical and scientific standards.
In accordance with the ethical standards set forth by the SciTeMed publishing group for the publication of high-quality scientific research, the author(s) of this article declare that there are no financial or other conflicts of interest that could potentially impact the integrity of the research presented. Additionally, the author(s) affirm that this work is solely the intellectual property of the author(s), and no other individuals or entities have substantially contributed to its content or findings.
It is imperative to acknowledge that the opinions and statements articulated in this article are the exclusive responsibility of the author(s), and do not necessarily reflect the views or opinions of their affiliated institutions, the publishing house, editors, or other reviewers. Furthermore, the publisher does not endorse or guarantee the accuracy of any statements made by the manufacturer(s) or author(s). These disclaimers emphasize the importance of respecting the author(s)' autonomy and the ability to express their own opinions regarding the subject matter, as well as those readers should exercise their own discretion in understanding the information provided. The position of the author(s) as well as their level of expertise in the subject area must be discerned, while also exercising critical thinking skills to arrive at an independent conclusion. As such, it is essential to approach the information in this article with an open mind and a discerning outlook.
© 2025 The Author(s). The article presented here is openly accessible under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). This license grants the right for the material to be used, distributed, and reproduced in any way by anyone, provided that the original author(s), copyright holder(s), and the journal of publication are properly credited and cited as the source of the material. We follow accepted academic practices to ensure that proper credit is given to the original author(s) and the copyright holder(s), and that the original publication in this journal is cited accurately. Any use, distribution, or reproduction of the material must be consistent with the terms and conditions of the CC-BY license, and must not be compiled, distributed, or reproduced in a manner that is inconsistent with these terms and conditions. We encourage the use and dissemination of this material in a manner that respects and acknowledges the intellectual property rights of the original author(s) and copyright holder(s), and the importance of proper citation and attribution in academic publishing.
Patients with gynecological abdominal wall malignancies can benefit significantly from radical resection and autologous reconstruction. The pedicled anterolateral thigh flap is the preferred donor site, offering a reliable solution to abdominal wall reconstruction in this setting. The satisfactory results should prompt a more aggressive surgical approach for these patients. This article describes the authors' experiences with the abdominal reconstruction following surgical resection of gynecological abdominal wall malignancy using pedicled anterolateral thigh flap.
The ALT and AMT flaps are the most commonly used thigh free flaps for intraoral reconstruction. Recently, PAP flap has been proposed as an alternative. This study aimed to compare the thickness of these thigh flaps and to identify the factors influencing flap thickness in our population.
A thin profunda artery perforator flap harvested from the left thigh is shown in this video. Preoperative computed tomographic angiography is used to assess morphology of the perforators and its branches, pedicle length and vertical location of the two branches from the ischial tuberosity. These measurements are translated on to the patient. Locations of both branches are confirmed with a handheld doppler. The authors concluded that preoperative computed tomographic angiography is a useful technique to provide detailed anatomic information on morphology of perforators, course through the septum or muscle above the deep fascia and skin thickness. Computed tomographic angiography allows quick and easy assessment of the whole vascular anatomy of the leg and helps to arrive at the decision about selection of the best flaps based on the characteristics of the defect and on the individual anatomy of the patient.
The senior author (Dr. Isao Koshima) designed a tibial osseo-periosteal (TOP) flap. TOP flap has a favorable anatomical position with a thin skin around it, hence it is a good option for an island flap. TOP flap can be used for various mild to moderately sized osteo-cutaneous defects with low morbidity. In this article, the authors describe their experience of the first reported cohort of TOP flaps in clinical practice.
The likelihood of donor site ischemia following the harvesting of a fibula flap is extremely low, but it is potentially lethal if it occurs. The authors describe a case of ischemia of the lower extremity following a free fibula harvest for head and neck reconstruction. The authors discuss preoperative, intraoperative, and postoperative strategies to assist in diagnosing and managing risks associated with free fibula flap harvesting in this paper.
The communication among international microsurgeons have switched from one direction (from paper, textbook) to multiway interactions through the internet. The authors believe the online platform will play an immensely important role in the learning and development in the field of microsurgery.
Traditionally, suturing techniques have been the mainstay for microvascular anastomoses, but owing to its technical difficulty and labour intensity, considerable work has gone into the development of sutureless microvascular anastomoses. In this review, the authors take a brief look at the developments of this technology through the years, with a focus on the more recent developments of laser-assisted vascular anastomoses, the unilink system, vascular closure staples, tissue adhesives, and magnets. Their working principles, with what has been found concerning their advantages and disadvantages are discussed.
Prof. Koushima, president of World Society for Reconstructive Microsurgery, proposes an innovative concept and technique of the multi-stage ‘Orochi’ combined flaps (sequential flaps in parallel). The technique opens a new vista in reconstructive microsurgery.
The video presents a useful technique for microvascular anastomosis in reconstructive surgery of the head and neck. It is advantageous to use this series of sutures when working with limited space, weak vessels (vessels irradiated, or with atheroclastic plaques), suturing in tension, or suturing smaller vessels (less than 0.8 cm in diameter).
Authors discuss a silicone tube that provides structural support to vessels throughout the entire precarious suturing process. This modification of the conventional microvascular anastomosis technique may facilitate initial skill acquisition using the rat model.
PEDs can be used as alternative means of magnification in microsurgery training considering that they are superior to surgical loupes in magnification, FOV and WD ranges, allowing greater operational versatility in microsurgical maneuvers, its behavior being closer to that of surgical microscopes in some optical characteristics. These devices have a lower cost than microscopes and some brands of surgical loupes, greater accessibility in the market and innovation plasticity through technological and physical applications and accessories with respect to classical magnification devices. Although PEDs own advanced technological features such as high-quality cameras and electronic loupes applications to improve the visualizations, it is important to continue the development of better technological applications and accessories for microsurgical practice, and additionally, it is important to produce evidence of its application at surgery room.
Avulsion injuries and replantation of the upper arm are particularly challenging in the field of traumatic microsurgery. At present, the functional recovery of the avulsion injuries upper arm after the replantation is generally not ideal enough, and there is no guideline for the surgeries. The aim of this study was to analyze the causes of failure of the upper arm replantation for avulsion injuries, summarize the upper arm replantation’s indications, and improve the replantation methods.
The supraclavicular flap has gained popularity in recent years as a reliable and easily harvested flap with occasional anatomical variations in the course of the pedicle. The study shows how the determination of the dominant pedicle may be aided with indocyanine green angiography. Additionally, the authors demonstrate how they convert a supraclavicular flap to a free flap if the dominant pedicle is unfavorable to a pedicled flap design.
The implications of rebound heparin hypercoagulability following cessation of therapy in microsurgery is unreported. In this article the authors report two cases of late digit circulatory compromise shortly after withdrawal of heparin therapy. The authors also propose potential consideration for changes in perioperative anticoagulation practice to reduce this risk.
In a cost-effective and portable way, a novel method was developed to assist trainees in spinal surgery to gain and develop microsurgery skills, which will increase self-confidence. Residents at a spine surgery center were assessed before and after training on the effectiveness of a simulation training model. The participants who used the training model completed the exercise in less than 22 minutes, but none could do it in less than 30 minutes previously. The research team created a comprehensive model to train junior surgeons advanced spine microsurgery skills. The article contains valuable information for readers.
The loupe plays a critical role in the microsurgeon's arsenal, helping to provide intricate details. In the absence of adequate subcutaneous fat, the prismatic lens of the spectacle model may exert enormous pressure on the delicate skin of the nasal bone. By developing a soft nasal support, the author has incorporated the principle of offloading into an elegant, simple yet brilliant innovation. A simple procedure such as this could prove invaluable for microsurgeons who suffer from nasal discoloration or pain as a result of prolonged use of prismatic loupes. With this technique, 42% of the pressure applied to the nose is reduced.
An examination of plastic surgery residents' experiences with microsurgery in Latin American countries was conducted in a cross-sectional study with 129 microsurgeons. The project also identifies ways to increase the number of trained microsurgeons in the region. The authors claim that there are few resident plastic surgeons in Latin America who are capable of attaining the level of experience necessary to function as independent microsurgeons. It is believed that international microsurgical fellowships would be an effective strategy for improving the situation.
This retrospective study on the keystone design perforator island flap (KDPIF) reconstruction offers valuable insights and compelling reasons for readers to engage with the article. By sharing clinical experience and reporting outcomes, the study provides evidence of the efficacy and safety profile of KDPIF as a reconstructive technique for soft tissue defects. The findings highlight the versatility, simplicity, and favorable outcomes associated with KDPIF, making it an essential read for plastic surgeons and researchers in the field. Surgeons worldwide have shown substantial interest in KDPIF, and this study contributes to the expanding knowledge base, reinforcing its clinical significance. Moreover, the study's comprehensive analysis of various parameters, including flap survival rate, complications, donor site morbidity, and scar assessment, enhances the understanding of the procedure's outcomes and potential benefits. The insights garnered from this research not only validate the widespread adoption of KDPIF but also provide valuable guidance for optimizing soft tissue reconstruction in diverse clinical scenarios. For readers seeking to explore innovative reconstructive techniques and improve patient outcomes, this article offers valuable knowledge and practical insights.
This comprehensive review article presents a profound exploration of critical facets within the realm of microsurgery, challenging existing paradigms. Through meticulous examination, the authors illuminate the intricate world of microangiosomes, dissection planes, and the clinical relevance of anatomical structures. Central to this discourse is an exhaustive comparative analysis of dermal plexus flaps, meticulously dissecting the viability and potential grafting applications of subdermal versus deep-dermal plexi. Augmenting this intellectual voyage are detailed illustrations, guiding readers through the intricate microanatomy underlying skin and adjacent tissues. This synthesis of knowledge not only redefines existing microsurgical principles but also opens new frontiers. By unearthing novel perspectives on microangiosomes and dissection planes and by offering a comparative insight into dermal plexus flaps, this work reshapes the landscape of microsurgery. These elucidations, coupled with visual aids, equip practitioners with invaluable insights for practical integration, promising to propel the field of microsurgery to unprecedented heights.
This article presents a groundbreaking surgical approach for treating facial paralysis, focusing on the combination of the pronator quadratus muscle (PQM) and the radial forearm flap (RFF). It addresses the challenges in restoring facial functions and skin closure in paralysis cases. The study's novelty lies in its detailed examination of the PQM's vascular anatomy when combined with the RFF, a topic previously unexplored. Through meticulous dissections, it provides crucial anatomical insights essential for enhancing facial reanimation surgeries, offering significant benefits in medical practices related to facial reconstruction and nerve transfer techniques.
This article exemplifies a significant advancement in microsurgical techniques, highlighting the integration of robotic-assisted surgery into the deep inferior epigastric perforator (DIEP) flap procedure for breast reconstruction. It demonstrates how innovative robotic technology refines traditional methods, reducing the invasiveness of surgeries and potentially lessening postoperative complications like pain and herniation by minimizing the length of the fascial incision. This manuscript is pivotal for professionals in the medical field, especially those specializing in plastic surgery, as it provides a comprehensive overview of the operative techniques, benefits, and critical insights into successful implementation. Moreover, it underscores the importance of ongoing research and adaptation in surgical practices to enhance patient outcomes. The article serves as a must-read, not only for its immediate clinical implications but also for its role in setting the stage for future innovations in robotic-assisted microsurgery.
The groundbreaking study illuminates the complex mechanisms of nerve regeneration within fasciocutaneous flaps through meticulous neurohistological evaluation, setting a new benchmark in experimental microsurgery. It challenges existing paradigms by demonstrating the transformative potential of sensory neurorrhaphy in animal models, suggesting possible clinical applications. The data reveal a dynamic interplay of nerve recovery and degeneration, offering critical insights that could revolutionize trauma management and reconstructive techniques. By bridging experimental findings with hypothetical clinical scenarios, this article inspires continued innovation and research, aimed at enhancing the efficacy of flap surgeries in restoring function and sensation, thus profoundly impacting future therapeutic strategies.
This article presents the first comprehensive review of refractory chylous ascites associated with systemic lupus erythematosus, analyzing 19 cases to propose an evidence-based therapeutic framework. It introduces lymphatic bypass surgery as an effective option for this rare complication, overcoming the limitations of conventional treatment. By integrating mechanical drainage, immunomodulation, and lymphangiogenesis, this approach achieves rapid and sustained resolution of ascites. The findings offer a novel surgical strategy for autoimmune lymphatic disorders and prompt a re-evaluation of their complex pathophysiology. This study demonstrates how surgical innovation can succeed where traditional therapies fail, offering new hope in managing refractory autoimmune disease.
Motorcycle chain-induced fingertip amputations represent a reconstructive dead end, where severe crushing and contamination traditionally compel revision amputation. The authors dismantle this exclusion criterion, reporting an 83% salvage rate using a modified protocol of radical debridement, strategic skeletal shortening, and simplified single-vessel supermicrosurgery. By eschewing complex grafting for tension-free primary anastomosis, the authors successfully restored perfusion in ostensibly
Division of the lateral plantar artery does not jeopardize the foot circulation because of anastomosis of the lateral plantar artery with the dorsalis pedis artery at the first intermetatarsal space. However, care should be taken with patients with peripheral artery occlusive disease and the flow of dorsalis pedis artery should be confirmed before surgery. Given the advantages of sizable vessel, easy dissection, and proximity to the defect, we believe that the lateral plantar artery might be a valuable option as recipient vessel for lateral plantar forefoot reconstruction.
The authors reviewed the MDCT images to show the number of lymph nodes superior to the saphenofemoral junction. In this study, on average, 3.67 nodes existed. However, there were 4 percent of cases with no countable nodes. This result indicates that appropriate preoperative screening is needed for this procedure.
The authors proposed a new less invasive island flap, namely the first metatarsal artery capillary perforator flap. The advantages of this flap include the preservation of the first metatarsal artery and the adiposal tissue in the web space, thereby preventing compression around the remaining deep peroneal nerve.
The ALT and AMT flaps are the most commonly used thigh free flaps for intraoral reconstruction. Recently, PAP flap has been proposed as an alternative. This study aimed to compare the thickness of these thigh flaps and to identify the factors influencing flap thickness in our population.
A thin profunda artery perforator flap harvested from the left thigh is shown in this video. Preoperative computed tomographic angiography is used to assess morphology of the perforators and its branches, pedicle length and vertical location of the two branches from the ischial tuberosity. These measurements are translated on to the patient. Locations of both branches are confirmed with a handheld doppler. The authors concluded that preoperative computed tomographic angiography is a useful technique to provide detailed anatomic information on morphology of perforators, course through the septum or muscle above the deep fascia and skin thickness. Computed tomographic angiography allows quick and easy assessment of the whole vascular anatomy of the leg and helps to arrive at the decision about selection of the best flaps based on the characteristics of the defect and on the individual anatomy of the patient.
The supraclavicular flap has gained popularity in recent years as a reliable and easily harvested flap with occasional anatomical variations in the course of the pedicle. The study shows how the determination of the dominant pedicle may be aided with indocyanine green angiography. Additionally, the authors demonstrate how they convert a supraclavicular flap to a free flap if the dominant pedicle is unfavorable to a pedicled flap design.
This retrospective study on the keystone design perforator island flap (KDPIF) reconstruction offers valuable insights and compelling reasons for readers to engage with the article. By sharing clinical experience and reporting outcomes, the study provides evidence of the efficacy and safety profile of KDPIF as a reconstructive technique for soft tissue defects. The findings highlight the versatility, simplicity, and favorable outcomes associated with KDPIF, making it an essential read for plastic surgeons and researchers in the field. Surgeons worldwide have shown substantial interest in KDPIF, and this study contributes to the expanding knowledge base, reinforcing its clinical significance. Moreover, the study's comprehensive analysis of various parameters, including flap survival rate, complications, donor site morbidity, and scar assessment, enhances the understanding of the procedure's outcomes and potential benefits. The insights garnered from this research not only validate the widespread adoption of KDPIF but also provide valuable guidance for optimizing soft tissue reconstruction in diverse clinical scenarios. For readers seeking to explore innovative reconstructive techniques and improve patient outcomes, this article offers valuable knowledge and practical insights.
This article exemplifies a significant advancement in microsurgical techniques, highlighting the integration of robotic-assisted surgery into the deep inferior epigastric perforator (DIEP) flap procedure for breast reconstruction. It demonstrates how innovative robotic technology refines traditional methods, reducing the invasiveness of surgeries and potentially lessening postoperative complications like pain and herniation by minimizing the length of the fascial incision. This manuscript is pivotal for professionals in the medical field, especially those specializing in plastic surgery, as it provides a comprehensive overview of the operative techniques, benefits, and critical insights into successful implementation. Moreover, it underscores the importance of ongoing research and adaptation in surgical practices to enhance patient outcomes. The article serves as a must-read, not only for its immediate clinical implications but also for its role in setting the stage for future innovations in robotic-assisted microsurgery.
This systematic review and meta-analysis provide a pragmatic evaluation of drain-free versus drain-based DIEP flap techniques for breast reconstruction, challenging the traditional reliance on drainage. By analyzing postoperative outcomes, the study highlights the potential for refining surgical strategies to enhance patient comfort and recovery without compromising safety. The findings offer a neutral perspective, suggesting that clinical practice may not necessarily depend on the use of drains. This revelation prompts medical professionals to reassess existing surgical approaches and may catalyze a paradigm shift in postoperative care. Presented with clear narrative and rigorous data analysis, the article encourages readers to consider the broader implications of surgical innovations on patient care protocols.
The authors present a study on bipedicled DIEP flap reconstruction for chest wall defects post-mastectomy, potentially advancing complex reconstructive techniques in breast cancer surgery with implications for improving patient outcomes. However, labeled as a "case series," the manuscript describes only one case, misaligning with case series standards requiring multiple cases. Major concerns include a superficial literature review failing to establish novelty, unspecified preoperative assessments, absent complication risk discussions, vague follow-up details, and lack of statistical analysis, undermining clinical applicability and rigor. In its current form, the manuscript does not meet publication standards. The authors should reclassify it as a case report, emphasizing qualitative insights, and address these critical flaws through substantial revisions to enhance clarity and credibility.
The authors present a novel approach to bipedicled DIEP flap reconstruction for post-mastectomy chest wall defects, offering valuable insights into donor-site preservation and potential improvements in functional and aesthetic outcomes. However, the manuscript lacks critical discussion of surgical complexity and risks, relies solely on subjective BREAST-Q scores without objective measures, provides limited comparison with alternative techniques, and omits key procedural details and figures (3–5), hindering reproducibility and clarity. These shortcomings compromise the manuscript’s rigor and clinical relevance, rendering it unsuitable for publication without substantial revision.
Gupta S, Arora R, Mishra KS, Kumar A, Prasad N. Reconstruction of massive chest wall defect after bilateral mastectomy using a bipedicled deep inferior epigastric perforator flap: A case report. Int Microsurg J 2025;9(1):3. https://doi.org/10.24983/scitemed.imj.2025.00198