Background: Avulsion injuries and replantation of the upper arm are particularly challenging in the field of traumatic microsurgery. At present, the functional recovery of the avulsion injuries upper arm after the replantation is generally not ideal enough, and there is no guideline for the surgeries. The aim of this study was to analyze the causes of failure of the upper arm replantation for avulsion injuries, summarize the upper arm replantation’s indications, and improve the replantation methods.
Methods: From January 2014 to January 2016, our department had treated 15 cases of trauma caused upper arm avulsion amputation injuries. All the injured arms had been replanted. We conducted rapid debridement, simple and effective external fixation, or internal fixation, and used microsurgical methods to repair blood vessels and nerves. After the surgery, the patients were prescribed medicines such as anti-inflammatory, anti-spasm, prophylactic antibiotics, anticoagulation, rehydration, and analgesic treatment. We also monitored patients’ blood supply situation closely.
Results: The 15 cases of the upper arm replantation for avulsion injuries resulted in a 100% postoperative patency rate, 73.3% skin necrosis rate, 60% muscle necrosis rate, and 20% amputation rate. Of all the cases, three cases were required to remove the replant limb due to unstable vital signs, acute renal failure, and major artery bleeding during the debridement. The average of the follow-up was two years. After one year of the operation, the replanted upper arm’s function was assessed according to the “Function score of upper limb replantation of Hand Surgery Society of Chinese Medical Association.” The average score was 25.2 points, which was classified as poor.
Conclusion: The upper arm avulsion injuries after trauma, which should have been treated with microsurgery, remains a challenging problem. There has been a lack of formed upper extremity replantation guide, and the patients are often hemodynamically unstable with multiple traumas and combined injuries, resulting in a high risk of failure. The long ischemia time often attributes to surgical failures and amputation. Skilled microsurgical techniques may improve the success rate of replantation.
Replantation of the avulsed upper arm is particularly challenging in the field of traumatic microsurgery. It is usually a high-level injury, severe soft tissue injury, and often combined with severe hemorrhagic shock and other complicated associate injuries which make the replantation a great risk. At present, the functional recovery of the avulsion injuries over upper arm after the replantation is generally not satisfied enough, and there is no guideline for the surgeries. There is still much controversy in this field [1,2].
On the other hand, the upper limb prostheses are not only expensive but also difficult to meet the needs of patients’ functional requirements. The upper limb prostheses are less useful than the lower extremity prostheses and the importance of replantation is still irreplaceable [3]. How to further clarify the indications for surgery, improve surgical techniques, and promote full recovery of patients with upper extremity function are still important issues in the field of limb replantation [4]. From January 2014 to January 2016, 15 cases of upper extremity avulsion injuries were treated in our department. Among them, three patients were amputated after the replantation surgery. The indications, surgical techniques, and rehabilitation methods of the replantation of the upper arm were discussed in this article.
General Information
There were 15 cases in this study, eleven males and four females. They were between 19-57 years old, with an average age of 35.8 years. Causes of injury include eight cases of machine injury, four cases of car accident, two cases of belt pulley injury, and one case of mixer injury. Injury sites include six cases of elbow, six cases of middle arm, and three cases of proximal arm. The ischemic time was 4-12 hours, an average of 6.26 hours. All patients suffered vascular and nerve defects. The defect length was 4-7 cm. Ten cases were performed shortening replantation and five cases were performed vascular graft replantation. Patients summary is shown in Table 1.
Surgical Methods
All the patients were operated under general anesthesia. Surgeons were divided into two teams and performed the following procedures concurrently. One team focused on the debridement, dissection, and marked the main vessels and nerves of the distal limb; and another team performed the same procedure on the proximal limb. The method of the surgery either shorten the limb for replant or transplant the vein graft to bridge the defect was decided according to the vessel defects, muscle, skin, and other soft tissue defects. If the fracture is comminuted and the skin, muscle defect is more than 5 cm, shorten limb replantation is selected. On the contrary, free blood vessel transplantation was chosen to replant the limbs. The average length of shortening of upper arm is 5 cm. For shortening replanted group, distal and proximal humeral shortening osteotomy were performed with the use of wire saw, then, a plate or external fixator was utilized to fix the broken ends. Under the microscope, the brachial artery and accompanying veins, cephalic vein, basilic vein were anastomosed, radial nerve, ulnar nerve, median nerve, and musculocutaneous nerve were copated, muscles were sutured to cover the vascular and nerves, placed drainage tube, and the skin closed. For non-shortening replanted group, the vein grafts and nerve graft required to bridge the defect. First, a plate or external fixator was used to quickly fix the broken ends, harvested the great saphenous vein from the contralateral lower limb, then bridged the brachial artery and anastomosed the major nerves, harvested the sural nerve from the contralateral lower limb, then bridged the major nerves. And anastomosed the cephalic vein and basilic vein, sutured muscle to cover the vessels and nerves, placed drainage tube, and sutured the skin. Skin necrosis and muscle necrosis were found to be the most common complications after the initial operation. Debridement and skin grafting were usually performed, some cases had vascular embolism, we performed the vessel transplantation for the patient.
Postoperative Management and Rehabilitation
After the replantation surgery, all patients were prescribed medicines including anti-inflammatory, anti-coagulant, anti-vasospasm, analgesic, vasodilator, transfusion, and rehydration therapy; ECG, blood oxygen saturation monitoring and blood pressure monitoring, review of the blood test, coagulation series, liver and kidney function tests, electrolytes and myocardial enzymes monitoring were also performed. The patients were completely bed ridden for seven days with limb warmth, no smoking, no mood swings, and changes in peripheral blood flow and skin temperature. After four weeks, the patients were required to move their fingers passively. After eight weeks, passive wrist and hand functional exercises, active shoulder, and elbow functional exercises were practiced. Different surgeries such as functional muscle, nerve, or tendons transfers were performed according to each patient’s condition during the functional recovery period. Three cases underwent nerve transfers and four cases underwent free tendons or functional muscle transfers. The four patients with elbow flexion dysfunction underwent functioning free gracilis muscle transplantation to reconstruct elbow joint function.
After the replantation surgery, doppler was used to explore the distal vascular patency and all the radial arteries of the patients could be detected. Vascular patency rate was 100%. Eleven patients had skin necrosis after the surgery; the incidence of skin necrosis was 73.3%. Nine patients had various muscle necroses; the incidence of muscle necrosis was 60%. A total of three patients were amputated; the amputation rate of patients was 20%. Elbow amputation is the osteotomy of the distal humerus to avoid the expand of the distal limb. One patient had avulsion of the upper arm and multiple ribs fractures. First day after the replantation surgery, the patient had elevated serum potassium, elevated myocardial enzymes, thrombocytopenia, coagulation disorders, and respiratory failure. An emergency amputation was performed; however, it did not save the patient’s life. One patient with acute renal failure was also amputated. One case was 20 days of discharge who had muscle necrosis; when debridement was done, the blood vessels were ruptured, and then he was amputated. Thirteen wound secretions were cultured after the operation and the infection rate was 86.7%. The patients were followed up for one to three years, with an average of two years. Upper limb function at one year after the replantation surgery was an average score of 25.2 points, which was considered poor function according to the Chinese Medical Association assessment criteria for upper limb amputation replantation (Table 2).
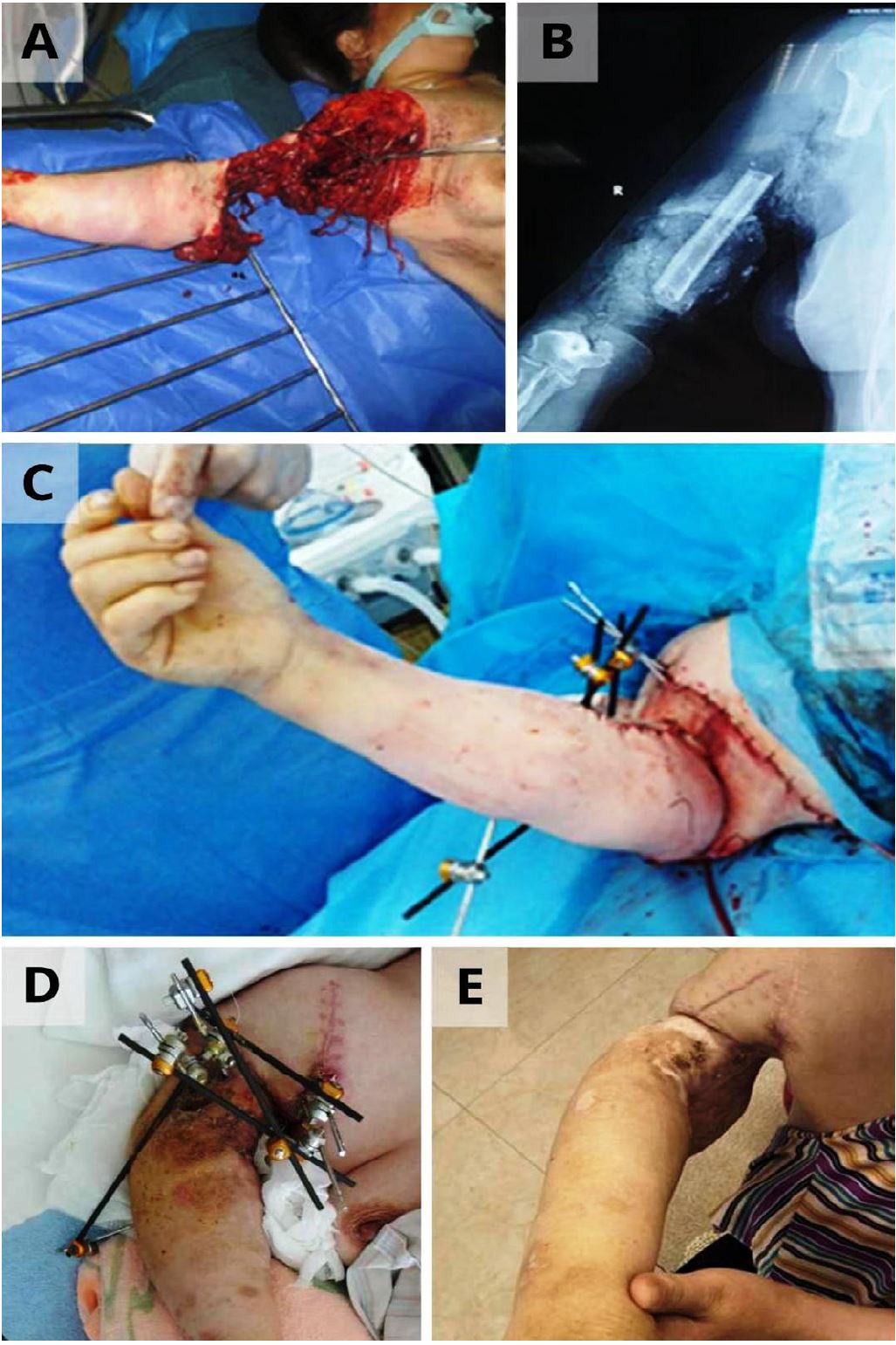
Figure 1. (A) Preoperative appearance. (B) Preoperative X-ray. (C) Postoperative appearance. (D) Four weeks after the replantation. (E) One year after the replantation.
Case Report
A 48 years old female was presented with a right upper arm avulsion injury caused by strangulation of the machine. The patient underwent shortening replanted surgery, and the limb was survived. The skin defect over axillary area was closed by the skin grafting, the outcome was satisfactory (Figure 1).
Upper Arm Avulsion and Replantation Indications
Avulsion injuries and replantation of the upper arm are particularly challenging in the field of traumatic microsurgery. Because avulsion injuries are usually high-level, severe soft tissue injuries, and often with severe hemorrhagic shock and other complex injuries. The replantation of upper arm possesses a great risk, and its indications in our institute include age below 60 years, no heart disease, hypertension, diabetes, or other underlying diseases, warm ischemia time is less than six hours, and without chest, abdomen, or head complex injury. The mangled extremity severity score (MESS) is one of the few scoring systems to predict limb salvage outcomes of upper extremity injures. However, MESS has been tested and found not very useful in several studies. The prevailing opinion is that in the upper extremity injury, every attempt should be made to salvage the limb. Another important indication is the will of the patient and his family. The contraindications of upper arm replantation in our institute include severe proximal arm avulsions or shoulder disarticulation with proximal nerve avulsion from brachial plexus nerves or roots [1].
Survival Analysis
After the replantation surgery of severed upper arm avulsion injury, the affected limb had a high rate of vascular patency; because of the thick upper arm vasculature, the collateral circulation was more abundant. However, 86.7% of the cases required secondary surgeries; the patients with muscle necrosis and infection underwent multiple debridement, the patients with skin necrosis received skin grafting, the patients with vascular embolism was performed vascular exploration, and the patients with limb necrosis and unstable vital signs required an emergency amputation. Due to severe skin and soft tissue contusion, the incidence of postoperative skin necrosis was 73.3%. The incidence of muscle necrosis was also high, 60%. Muscle ischemia-resistant time was 6 hours, for the patient injured to the recanalization of the blood vessels usually needed more than 6 hours. After recanalization, although the limbs could be saved, the muscle necrosis was inevitable. The consequent wound infection was also inevitable. Among the group of 15 cases of replantation patients, three patients were performed the amputation surgery, the amputation rate was 20%. Among the three patients who received amputations. One patient died of upper limb avulsion after the replantation surgery. The patient was male, 25 years old, who was admitted to the hospital with bilateral upper extremities avulsion injuries, bilateral clavicle fracture, bilateral scapular fracture, and bilateral multiple rib fractures. The patient had elevated serum potassium, elevated myocardial enzymes, thrombocytopenia, coagulation disorders, and respiratory failure on the first day after the replantation surgery. We did the emergency amputation, but the patient was still dead. One patient had acute renal failure, creatine kinase was 17000u / L, persistent fever, confusion, and we did the emergency amputation surgery for him. One patient was discharged 10 days after the operation and transferred to a lower hospital for treatment. During the procedure of dressing change, the brachial artery was injured. On the 20th day after the operation, the limb of the patient with devascularization was replanted and returned to our hospital again. After exploration, muscle necrosis and peripheral devascularization were found in the affected limb, and finally, amputation was performed. With the development of microsurgery, the success rate of vascular anastomosis had been very high in traumatic micro-orthopedics in the case of the vascular graft after severed wounds in the large limbs. However, patients often suffered more injuries. To increase the success of the replantation, at the beginning of the surgery, we used a tube to connect the main artery for shunting to reduce the ischemic time of the severed limb.
Factors Influencing the Survival Rate
For patients with stable vital signs, no fatal composite injury was the primary condition for limb survival. On the other hand, one patient in this study had severe upper arm avulsion, and other injuries include bilateral scapula, clavicle fractures, and multiple fractures of the ribs. The patient died from severe complications after the replantation surgery. Preoperative detailed physical examination was necessary to avoid unfavorable postoperative outcomes, and the patients needed relevant departments’ consultation; and lifesaving should be considered priority before limb salvage. The quality of vascular anastomosis was also an important factor for the survival of replantation limbs. Because of the long segment of blood vessel contusion and avulsion, the plane of vascular injury was difficult to judge. Surgeons must judge the length of the vascular defect accurately. Before the shortening replantation or vascular graft replantation, we used catheter shunting surgery to provide the blood supply of the distal limb, which could greatly shorten the time of muscle ischemia and prevent future muscle tissue necrosis, leading to a better postoperative function recovery and significantly improving the survival rate of replantation and muscle necrosis.
The Replantation Limb Function Recovery
Patients with upper limb avulsion and replantation generally had poor functional recovery after transplantation. Although most of the patients had their nerves repaired during operation, the postoperative functional recovery was extremely limited due to the nerve avulsion. Because of the longtime of muscle ischemia after replantation of avulsion injury of the upper arm, which will lead to muscle fibrosis and even necrosis, we suggest that the catheter should be used to open the blood of the distal limb for the first time, so as to minimize the ischemic time of the distal limb. In addition, the avulsed nerve should be repaired as early as possible. If the nerve was damaged, nerve transplantation can be carried out early, so that the function of the severed limb can be restored to the greatest extent. After replantation, the early passive activities also play an important role in the recovery of limb function. The time of 4-8 weeks after the surgery is a critical period of rehabilitation. In this period, the patients may have consequences such as the upper extremity external fixation not maintaining a safe position, many scar formations, or joint stiffness which make the patients lost conditions of rehabilitation and reconstruction. During this period patients should pay attention to continue to maintain the function of the upper limb and hand. The hand and the wrist should do passive activities, the shoulder and the elbow should begin to do an initiative activity with protection. Eight weeks after surgery, most of the wounds have been healed. After two years, with effective rehabilitation training, the function of the upper arm will have reconstruction. This period the patients should be unswervingly encouraged to build confidence in life and with functional reconstruction [6]. Although successful replantation is a great comfort for the patient's psychology, the loss of long-term function makes the patient's psychological expectation declining gradually. Difficult to return to the original job again, the fight against the patient's family is still huge.
Upper arm avulsion injuries after trauma remains a challenging problem, and it requires a treatment with microsurgery. There has been a lack of formed upper extremity replantation guide, and the patients are often hemodynamically unstable with multiple traumas and combined injuries, resulting in a high risk of replantation. The long waiting time from injury to inadequate blood flow often attributes to surgical failures and amputation. Skilled microsurgical techniques may improve the success rate of replantation.
Received date: November 15, 2019
Accepted date: August 02, 2020
Published date: September 08, 2020
This article was presented at the 10th Congress of World Society for Reconstructive Microsurgery, in Bologna, Italy, in 2019.
The study is in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
The study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors report no financial or other conflict of interest relevant to this article, which is the intellectual property of the authors.
© 2020 The Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY).
The communication among international microsurgeons have switched from one direction (from paper, textbook) to multiway interactions through the internet. The authors believe the online platform will play an immensely important role in the learning and development in the field of microsurgery.
Traditionally, suturing techniques have been the mainstay for microvascular anastomoses, but owing to its technical difficulty and labour intensity, considerable work has gone into the development of sutureless microvascular anastomoses. In this review, the authors take a brief look at the developments of this technology through the years, with a focus on the more recent developments of laser-assisted vascular anastomoses, the unilink system, vascular closure staples, tissue adhesives, and magnets. Their working principles, with what has been found concerning their advantages and disadvantages are discussed.
Prof. Koushima, president of World Society for Reconstructive Microsurgery, proposes an innovative concept and technique of the multi-stage ‘Orochi’ combined flaps (sequential flaps in parallel). The technique opens a new vista in reconstructive microsurgery.
The video presents a useful technique for microvascular anastomosis in reconstructive surgery of the head and neck. It is advantageous to use this series of sutures when working with limited space, weak vessels (vessels irradiated, or with atheroclastic plaques), suturing in tension, or suturing smaller vessels (less than 0.8 cm in diameter).
Authors discuss a silicone tube that provides structural support to vessels throughout the entire precarious suturing process. This modification of the conventional microvascular anastomosis technique may facilitate initial skill acquisition using the rat model.
PEDs can be used as alternative means of magnification in microsurgery training considering that they are superior to surgical loupes in magnification, FOV and WD ranges, allowing greater operational versatility in microsurgical maneuvers, its behavior being closer to that of surgical microscopes in some optical characteristics. These devices have a lower cost than microscopes and some brands of surgical loupes, greater accessibility in the market and innovation plasticity through technological and physical applications and accessories with respect to classical magnification devices. Although PEDs own advanced technological features such as high-quality cameras and electronic loupes applications to improve the visualizations, it is important to continue the development of better technological applications and accessories for microsurgical practice, and additionally, it is important to produce evidence of its application at surgery room.
The supraclavicular flap has gained popularity in recent years as a reliable and easily harvested flap with occasional anatomical variations in the course of the pedicle. The study shows how the determination of the dominant pedicle may be aided with indocyanine green angiography. Additionally, the authors demonstrate how they convert a supraclavicular flap to a free flap if the dominant pedicle is unfavorable to a pedicled flap design.
The implications of rebound heparin hypercoagulability following cessation of therapy in microsurgery is unreported. In this article the authors report two cases of late digit circulatory compromise shortly after withdrawal of heparin therapy. The authors also propose potential consideration for changes in perioperative anticoagulation practice to reduce this risk.
In a cost-effective and portable way, a novel method was developed to assist trainees in spinal surgery to gain and develop microsurgery skills, which will increase self-confidence. Residents at a spine surgery center were assessed before and after training on the effectiveness of a simulation training model. The participants who used the training model completed the exercise in less than 22 minutes, but none could do it in less than 30 minutes previously. The research team created a comprehensive model to train junior surgeons advanced spine microsurgery skills. The article contains valuable information for readers.
The loupe plays a critical role in the microsurgeon's arsenal, helping to provide intricate details. In the absence of adequate subcutaneous fat, the prismatic lens of the spectacle model may exert enormous pressure on the delicate skin of the nasal bone. By developing a soft nasal support, the author has incorporated the principle of offloading into an elegant, simple yet brilliant innovation. A simple procedure such as this could prove invaluable for microsurgeons who suffer from nasal discoloration or pain as a result of prolonged use of prismatic loupes. With this technique, 42% of the pressure applied to the nose is reduced.
An examination of plastic surgery residents' experiences with microsurgery in Latin American countries was conducted in a cross-sectional study with 129 microsurgeons. The project also identifies ways to increase the number of trained microsurgeons in the region. The authors claim that there are few resident plastic surgeons in Latin America who are capable of attaining the level of experience necessary to function as independent microsurgeons. It is believed that international microsurgical fellowships would be an effective strategy for improving the situation.
This retrospective study on the keystone design perforator island flap (KDPIF) reconstruction offers valuable insights and compelling reasons for readers to engage with the article. By sharing clinical experience and reporting outcomes, the study provides evidence of the efficacy and safety profile of KDPIF as a reconstructive technique for soft tissue defects. The findings highlight the versatility, simplicity, and favorable outcomes associated with KDPIF, making it an essential read for plastic surgeons and researchers in the field. Surgeons worldwide have shown substantial interest in KDPIF, and this study contributes to the expanding knowledge base, reinforcing its clinical significance. Moreover, the study's comprehensive analysis of various parameters, including flap survival rate, complications, donor site morbidity, and scar assessment, enhances the understanding of the procedure's outcomes and potential benefits. The insights garnered from this research not only validate the widespread adoption of KDPIF but also provide valuable guidance for optimizing soft tissue reconstruction in diverse clinical scenarios. For readers seeking to explore innovative reconstructive techniques and improve patient outcomes, this article offers valuable knowledge and practical insights.
This comprehensive review article presents a profound exploration of critical facets within the realm of microsurgery, challenging existing paradigms. Through meticulous examination, the authors illuminate the intricate world of microangiosomes, dissection planes, and the clinical relevance of anatomical structures. Central to this discourse is an exhaustive comparative analysis of dermal plexus flaps, meticulously dissecting the viability and potential grafting applications of subdermal versus deep-dermal plexi. Augmenting this intellectual voyage are detailed illustrations, guiding readers through the intricate microanatomy underlying skin and adjacent tissues. This synthesis of knowledge not only redefines existing microsurgical principles but also opens new frontiers. By unearthing novel perspectives on microangiosomes and dissection planes and by offering a comparative insight into dermal plexus flaps, this work reshapes the landscape of microsurgery. These elucidations, coupled with visual aids, equip practitioners with invaluable insights for practical integration, promising to propel the field of microsurgery to unprecedented heights.
This article presents a groundbreaking surgical approach for treating facial paralysis, focusing on the combination of the pronator quadratus muscle (PQM) and the radial forearm flap (RFF). It addresses the challenges in restoring facial functions and skin closure in paralysis cases. The study's novelty lies in its detailed examination of the PQM's vascular anatomy when combined with the RFF, a topic previously unexplored. Through meticulous dissections, it provides crucial anatomical insights essential for enhancing facial reanimation surgeries, offering significant benefits in medical practices related to facial reconstruction and nerve transfer techniques.
This article exemplifies a significant advancement in microsurgical techniques, highlighting the integration of robotic-assisted surgery into the deep inferior epigastric perforator (DIEP) flap procedure for breast reconstruction. It demonstrates how innovative robotic technology refines traditional methods, reducing the invasiveness of surgeries and potentially lessening postoperative complications like pain and herniation by minimizing the length of the fascial incision. This manuscript is pivotal for professionals in the medical field, especially those specializing in plastic surgery, as it provides a comprehensive overview of the operative techniques, benefits, and critical insights into successful implementation. Moreover, it underscores the importance of ongoing research and adaptation in surgical practices to enhance patient outcomes. The article serves as a must-read, not only for its immediate clinical implications but also for its role in setting the stage for future innovations in robotic-assisted microsurgery.
The groundbreaking study illuminates the complex mechanisms of nerve regeneration within fasciocutaneous flaps through meticulous neurohistological evaluation, setting a new benchmark in experimental microsurgery. It challenges existing paradigms by demonstrating the transformative potential of sensory neurorrhaphy in animal models, suggesting possible clinical applications. The data reveal a dynamic interplay of nerve recovery and degeneration, offering critical insights that could revolutionize trauma management and reconstructive techniques. By bridging experimental findings with hypothetical clinical scenarios, this article inspires continued innovation and research, aimed at enhancing the efficacy of flap surgeries in restoring function and sensation, thus profoundly impacting future therapeutic strategies.
This article presents the first comprehensive review of refractory chylous ascites associated with systemic lupus erythematosus, analyzing 19 cases to propose an evidence-based therapeutic framework. It introduces lymphatic bypass surgery as an effective option for this rare complication, overcoming the limitations of conventional treatment. By integrating mechanical drainage, immunomodulation, and lymphangiogenesis, this approach achieves rapid and sustained resolution of ascites. The findings offer a novel surgical strategy for autoimmune lymphatic disorders and prompt a re-evaluation of their complex pathophysiology. This study demonstrates how surgical innovation can succeed where traditional therapies fail, offering new hope in managing refractory autoimmune disease.
This case highlights the use of a bipedicled deep inferior epigastric perforator (DIEP) flap for reconstructing a massive 45 × 17 cm chest wall defect following bilateral mastectomy. By preserving abdominal musculature and utilizing preoperative computed tomographic angiography (CTA) for perforator mapping, the technique enabled tension-free bilateral microvascular anastomosis to the internal mammary arteries. The incorporation of submuscular mesh and minimal donor-site undermining maintained abdominal wall integrity. At six-month follow-up, no hernia or functional deficits were observed, and the patient reported high satisfaction on the BREAST-Q. This muscle-sparing strategy offers a viable alternative for large, midline-crossing chest wall defects where conventional flaps may be insufficient.
Motorcycle chain-induced fingertip amputations represent a reconstructive dead end, where severe crushing and contamination traditionally compel revision amputation. The authors dismantle this exclusion criterion, reporting an 83% salvage rate using a modified protocol of radical debridement, strategic skeletal shortening, and simplified single-vessel supermicrosurgery. By eschewing complex grafting for tension-free primary anastomosis, the authors successfully restored perfusion in ostensibly
The main topic is relevant for the area of reconstructive microsurgery, focusing in a particularly challenging situation as is the major upper limb replantation in cases of traction- avulsion amputation at proximal level. Presenting a good number of cases (17) in a short period of time (2014-2016). The manuscript is overall well-presented, but revisions are required. The recommended revisions are summarized as follows.
Du X, Liu Y, Ou X, Xiong Y, Cong F, Liu Y, Song T. Survival analysis of upper arm replantation after avulsion injuries. Int Microsurg J 2020;4(1):4. https://doi.org/10.24983/scitemed.imj.2020.00135