In surgical procedures involving the penopubic junction, there are significant risks associated with postoperative scar traction. Scar traction may result in a short penis and other deformities, which may cause discomfort during erections and interfere with the patient's sexual performance. The article describes the case of a 27-year-old male who had undergone a penis lengthening procedure four years earlier. After the surgery, the skin around the penopubic junction was scarred and became severely contracted. This led to a short penis and a high hanging scrotum as a consequence of the scarring. The purpose of this case report is to describe how we repaired the penopubic junction with a pedicled superficial circumflex iliac artery perforator flap. At the penopubic junction, there was a defect measuring 4 x 3 cm following the removal of the contracture scar. The affected region was repaired using a left pedicled modified superficial circumflex iliac artery perforator flap based on its medial superficial branch. Moreover, a hybrid technique was developed to harvest the superficial circumflex iliac artery perforator flap in a safe and effective manner. Using the hybrid technique, a proximal-to-distally flap elevation approach was combined with a pedicle elongation strategy to lengthen the pedicle. It is our experience that the pedicled superficial circumflex iliac artery perforator flap may provide an effective alternative method of reconstructing the postoperative scar traction at the penopubic junction.
Postoperative scar traction is a potential complication of surgery involving the penopubic junction. An individual with scar traction at the penopubic junction may have a short penis and other deformities, which may affect his sexual performance and cause discomfort during erections. Research has shown that penopubic defects can be repaired using skin grafts, locoregional flaps, or microsurgical free tissue transfers [1-9]. However, despite the fact that each of these options has its own advantages and disadvantages, there is still considerable uncertainty regarding the most effective method of reconstructing penopubic defects. Therefore, research is underway to develop a practical and improved method of treating postoperative scar contractures of the penopubic region.
The superficial circumflex iliac artery perforator (SCIP) flap has been described by Koshima et al. as a feasible option for the reconstruction of limb deformities [10]. The SCIP flaps are thin, pliable, and versatile flaps with the advantage of minimal donor-site morbidity and well-concealed donor scarring. It should be noted, however, that the SCIP flap has a limited pedicle length, making it unsuitable for a broad range of applications. It is recommended that the maximum flap size be in the range of 10 x 30 cm, while the pedicle length may vary within the range of 20 cm. In the meantime, the SCIP flap can be constructed according to the Orochi technique [11], which includes the iliac bone for the reconstruction of the bone defect, the lateral femoral cutaneous nerve for a sensate flap, the fascia for the reconstruction of the tendons, and the sartorius muscle for the reconstruction of dynamic function.
Our main objective in this case report is to explore modifications to the SCIP flap in order to broaden its potential applications. A specific focus of this research is on the SCIP flap as an alternative reconstruction option for defects of the penopubic junction. In this case report, we illustrate how we have developed a hybrid technique to facilitate the elevation of the SCIP flap and overcome its major disadvantage, which is its short pedicle length. In this hybrid technique, the proximal-to-distally flap elevation approach [12] was combined with an elongation strategy that modifies the pedicle length [13].
We present the case of a 27-year-old male patient who underwent penis lengthening surgery four years ago. A severe postoperative complication occurred as a result of scar contracture at the penopubic junction, leading to a short penis and high hanging scrotum (Figure 1A). While the patient reported tightness during erections, there was no apparent effect on the performance of his sexual function due to the condition.
An appropriate surgical procedure was devised for resolving the scar contracture at the penopubic junction. A preliminary examination was conducted to identify the anterior superior iliac spine and pubic tubercle. A handheld doppler was used to mark the alignment of the superficial branch of the superficial circumflex iliac artery preoperatively. This branch traveled in an axial pattern beyond the anterior superior iliac spine (Figure 1B).
A contracture scar measuring 4 x 3 cm was excised at the penopubic junction (Figure 1C). A medial inferior incision was initially made as an exploratory procedure. Once the pedicle was identified, the skin paddle was redesigned laterally using a freestyle technique, and subsequent intrasubcutaneous dissections were performed under a microscope. The pedicle measured 7 cm in length (Figure 1D).
An appropriate flap was transposed through a subcutaneous tunnel and tailored to fit the defect. The defect in the penopubic junction was therefore reconstructed using a left pedicled modified SCIP flap based on the medial superficial branch (Figure 1E). During the surgical procedure, special care was taken to ensure the preservation of the dorsal nerve of the penis and the left iliohypogastric nerve. A primary wound closure was performed at the donor site. Overall, the duration of the surgery was 120 minutes, which included 45 minutes for flap harvesting. Postoperative recovery was uneventful for the patient after 1 month (Figure 1F) and 3 months (Figure 1G).
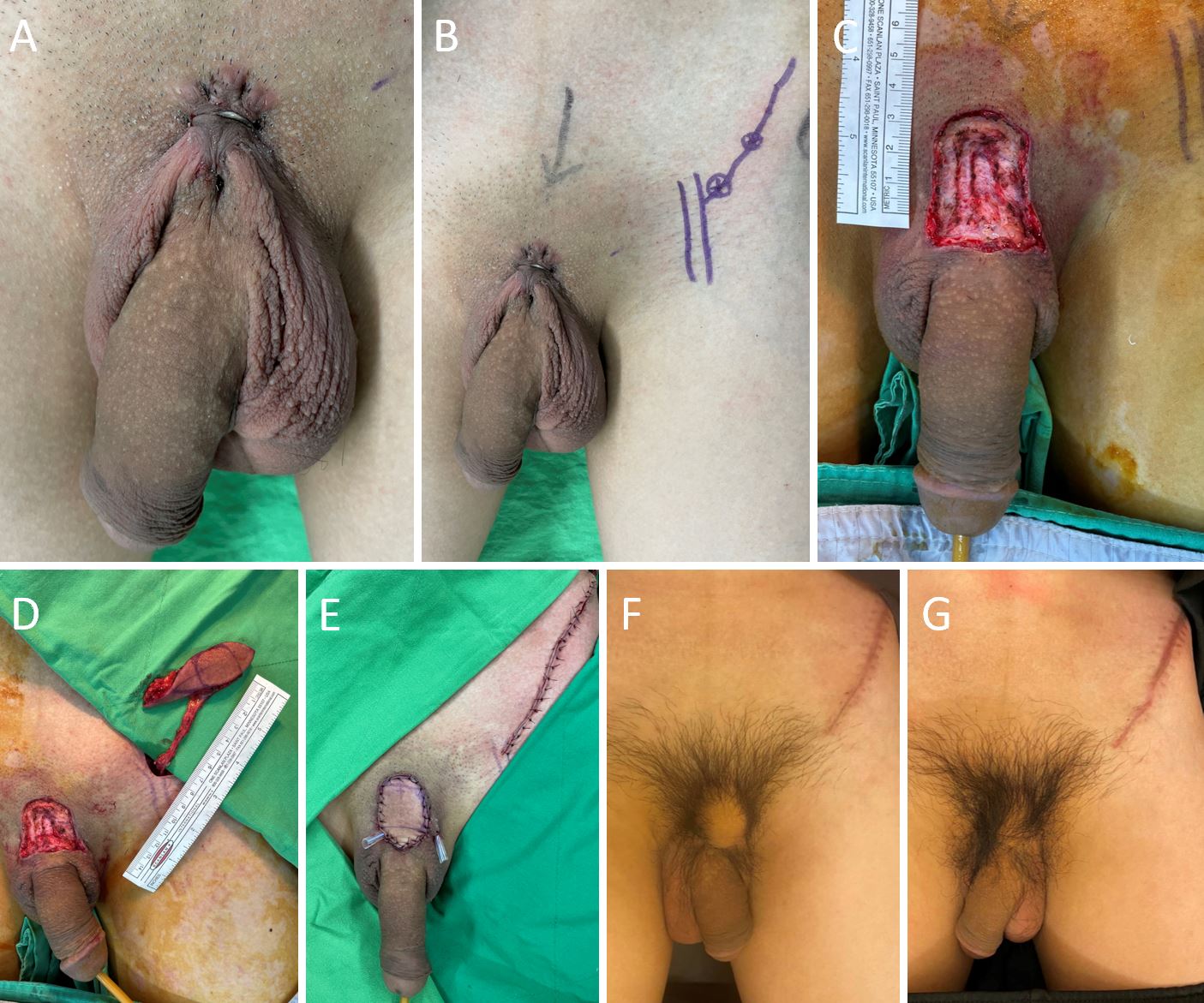
Figure 1. A 27-year-old male with a severe scar contracture at the penopubic junction. (A) Due to the scar contracture at the penopubic junction, there is a short penis and a high hanging scrotum. (B) A handheld doppler is used to determine the direction of the superficial branch of the superficial circumflex iliac artery. This branch travels beyond the anterior superior iliac spine in an axial pattern. (C) Following the excision of the contracture scar, there is a defect measuring 4 x 3 cm. (D) The length of the pedicle is 7 cm. (E) The flap is transpositioned through a subcutaneous tunnel and then tailored to fit the defect. At the donor site, a primary wound closure is performed. (F) One month after surgery, the patient recovers uneventfully. (G) The flap with hair growth is viable and durable three months after surgery.
Using a hybrid technique, we were able to safely harvest the SCIP flap and effectively overcome its major disadvantage, which was its short pedicle length. With the SCIP flap used to restore the penopubic area, excessive tension was minimized following scar contracture release. Our study expands the potential applications of the SCIP flap by employing it to reconstruct the postoperative scar traction at the penopubic junction. Our experience indicates that the long pedicle SCIP flap can be used as an alternative single-stage operation with satisfactory outcomes.
A variety of methods are available for the reconstruction of defects in the pubic or penopubic areas, such as using skin grafts, locoregional flaps, and microsurgical free tissue transfers [1-9]. A local flap is an advantageous method of reconstructing the penopubic area since it allows color matching and hair bearing. Local flaps can be employed in various ways, including the local iliac flap, the rhomboid flap from the suprapubic region, as well as the V-Y advancement flap [1-3].
A concern associated with using skin grafts or local flaps is the possibility of scar contracture recurrence, especially if the patient previously had hypertrophic scarring or keloids. Revision surgery may then be required in order to correct the problem [3]. In the case of skin grafting, a two-stage operation with dermal substitute combined with foreskin or hair bearing skin grafts is a viable alternative to minimize the risk of scar contracture recurrence, whereas direct skin grafting limits the treatment options for scarred wound beds.
Various regional flaps are commonly used, such as the scrotal flap, the groin flap, the deep external pudendal artery perforator flap, and the pudendal artery perforator flap [3-6]. Regional flaps have several shortcomings, including hairless patches or a mismatch in color. However, the bald patch can be combed with pubic hair or secondary hair transplantation with a micrograft or follicular unit graft. In the case of penopubic junction reconstruction using a pedicle SCIP flap, there is the disadvantage of leaving behind a non-sensate area and the possibility of creating hypertrophic scarring. Nevertheless, it is possible for the sensation to gradually return, and scars can also be treated with Z-plasty.
Several studies have demonstrated that microsurgical free tissue transfers are a viable option for reconstructing defects in the pubic or penopubic regions [7-9]. Different types of free tissue transfers exist, including the hair bearing expanded free forehead flap and the hair bearing temporoparietal flap based on superficial temporal vessels with or without needle epilation [7-9]. However, microsurgical free tissue transfers are time-consuming when attempting to reconstruct pubic or penopubic defects.
The importance of this research lies in expanding the scope of application of the SCIP flap by using it to reconstruct postoperative scar traction at the penopubic junction. Additionally, our research contributes to the development of a hybrid technique to facilitate the elevation of the SCIP flap and overcome its main disadvantage, namely its short pedicle length. The hybrid technique incorporates a proximal-to-distally elevation method [12] combined with an elongation strategy that modifies the pedicle length [13].
The proximal-to-distally flap elevation technique was first described by Yoshimatsu et al. [12]. In this procedure, a SCIP flap is elevated by identifying the pedicle arteries in order to incorporate a variety of anatomical structures. A major advantage of this proximal-to-distal elevation is that when the superficial branch of the superficial circumflex iliac artery is inadequate or not present, the pedicle can be switched to the deep branch of the superficial circumflex iliac artery or even to the superficial inferior epigastric artery.
The main disadvantage of the SCIP flap is the short pedicle length. Kwon et al. detailed the modification of SCIP flap elevation to obtain long pedicles using a laterally designed flap in conjunction with an intrasubcutaneous dissection [13]. With the long pedicle of the SCIP flap, the pedicle can be prevented from being twisted by a superficial band during inguinal transposition. In addition, lymphedema in the contralateral groin area can be reconstructed by including a lymphatic channel in the flap.
Using the proximal-to-distally elevation technique [12] in combination with the elongation strategy that modifies the pedicle length [13], we contribute to the development of a hybrid technique. It is our belief that a hybrid harvesting technique would make flap harvesting both safer and more flexible.
The use of pedicled SCIP flaps may provide an alternative reconstruction method for addressing scar traction at the penopubic junction following surgery. The procedure has demonstrated effectiveness for surgeons, as well as satisfactory results for patients.
Received date: April 01, 2022
Accepted date: May 18, 2022
Published date: August 18, 2022
The manuscript has not been presented at any meetings on the topic.
The study is in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The authors obtained permission from the participants in the human research prior to publishing their images or photographs.
This research has received no specific grant from any funding agency either in the public, commercial, or not-for-profit sectors.
There are no conflicts of interest declared by either the authors or the contributors of this article, which is their intellectual property.
It should be noted that the opinions and statements expressed in this article are those of the respective author(s) and are not to be regarded as factual statements. These opinions and statements may not represent the views of their affiliated organizations, the publishing house, the editors, or any other reviewers since these are the sole opinion and statement of the author(s). The publisher does not guarantee or endorse any of the statements that are made by the manufacturer of any product discussed in this article, or any statements that are made by the author(s) in relation to the mentioned product.
© 2022 The Author(s). This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). In accordance with accepted academic practice, anyone may use, distribute, or reproduce this material, so long as the original author(s), the copyright holder(s), and the original publication of this journal are credited, and this publication is cited as the original. To the extent permitted by these terms and conditions of license, this material may not be compiled, distributed, or reproduced in any manner that is inconsistent with those terms and conditions.
Video 1. Conversations with SciTeMed Editors and Expert Mentors.
Division of the lateral plantar artery does not jeopardize the foot circulation because of anastomosis of the lateral plantar artery with the dorsalis pedis artery at the first intermetatarsal space. However, care should be taken with patients with peripheral artery occlusive disease and the flow of dorsalis pedis artery should be confirmed before surgery. Given the advantages of sizable vessel, easy dissection, and proximity to the defect, we believe that the lateral plantar artery might be a valuable option as recipient vessel for lateral plantar forefoot reconstruction.
Health care systems in many countries are confronted with increasing economic limitations. Thus, complex microsurgical procedures and extensive rehabilitation programs are poorly compensated. However, this case demonstrates a dramatic reduction of socioeconomic expenses by allowing a potential radiocarpal amputee to return to work for another estimated 30 years.
Pedicled anterolateral thigh flap is a versatile option for reconstruction of complex soft tissue defects in varied anatomical regions. Its wide arc of rotation and less donor site morbidity are its added advantages.
The authors reviewed the MDCT images to show the number of lymph nodes superior to the saphenofemoral junction. In this study, on average, 3.67 nodes existed. However, there were 4 percent of cases with no countable nodes. This result indicates that appropriate preoperative screening is needed for this procedure.
Supraclavicular flap is an excellent fasciocutaneous flap for head and neck reconstruction due to its close color and texture match. In general, long flaps are required, but with the risk of distal necrosis. The aim of this study is to assess the relationship between the length and distal end necrosis of the supraclavicular flap.
The authors describe various patient and breast-related factors that influence surgical outcomes while also addressing some techniques and principles for aesthetic microsurgical reconstruction.
The authors present a retrospective review of 7 patients who underwent wide excision of the malignant tumors around the clavicle. Patient demographics, clinical details, the arc of rotation, outcome, and complications were analyzed.
The authors proposed a new less invasive island flap, namely the first metatarsal artery capillary perforator flap. The advantages of this flap include the preservation of the first metatarsal artery and the adiposal tissue in the web space, thereby preventing compression around the remaining deep peroneal nerve.
Prof. Koushima, president of World Society for Reconstructive Microsurgery, proposes an innovative concept and technique of the multi-stage ‘Orochi’ combined flaps (sequential flaps in parallel). The technique opens a new vista in reconstructive microsurgery.
The senior author (Dr. Isao Koshima) designed a tibial osseo-periosteal (TOP) flap. TOP flap has a favorable anatomical position with a thin skin around it, hence it is a good option for an island flap. TOP flap can be used for various mild to moderately sized osteo-cutaneous defects with low morbidity. In this article, the authors describe their experience of the first reported cohort of TOP flaps in clinical practice.
The authors present a revised application of the composite iliac crest bone free flap for hemimaxillectomy defects. This flap solely can give a support to the eye globe and the dental implants without osteotomies and titanium meshes. The upper ridge of the flap can be shaped to replicate the curvature of the orbital floor. The inner oblique muscle and the deep fascia can serve as an additional material for separation of the oral cavity from the nasal airway. Utilization of the Customized Contour Implants gives a surgeon a refining instrument for aesthetic correction of facial projection.
Patients with gynecological abdominal wall malignancies can benefit significantly from radical resection and autologous reconstruction. The pedicled anterolateral thigh flap is the preferred donor site, offering a reliable solution to abdominal wall reconstruction in this setting. The satisfactory results should prompt a more aggressive surgical approach for these patients. This article describes the authors' experiences with the abdominal reconstruction following surgical resection of gynecological abdominal wall malignancy using pedicled anterolateral thigh flap.
The ALT and AMT flaps are the most commonly used thigh free flaps for intraoral reconstruction. Recently, PAP flap has been proposed as an alternative. This study aimed to compare the thickness of these thigh flaps and to identify the factors influencing flap thickness in our population.
A thin profunda artery perforator flap harvested from the left thigh is shown in this video. Preoperative computed tomographic angiography is used to assess morphology of the perforators and its branches, pedicle length and vertical location of the two branches from the ischial tuberosity. These measurements are translated on to the patient. Locations of both branches are confirmed with a handheld doppler. The authors concluded that preoperative computed tomographic angiography is a useful technique to provide detailed anatomic information on morphology of perforators, course through the septum or muscle above the deep fascia and skin thickness. Computed tomographic angiography allows quick and easy assessment of the whole vascular anatomy of the leg and helps to arrive at the decision about selection of the best flaps based on the characteristics of the defect and on the individual anatomy of the patient.
The supraclavicular flap has gained popularity in recent years as a reliable and easily harvested flap with occasional anatomical variations in the course of the pedicle. The study shows how the determination of the dominant pedicle may be aided with indocyanine green angiography. Additionally, the authors demonstrate how they convert a supraclavicular flap to a free flap if the dominant pedicle is unfavorable to a pedicled flap design.
Smartphones and cellular technology have revolutionized flap monitoring. Smartphones provide low-cost thermal imaging alternatives to flap monitoring. It remains unclear, however, whether this method is accurate or reliable. It may be challenging to use smartphone thermal imaging when clinicians fail to communicate clinically relevant events. The authors demonstrate three instances in which the thermal imaging information on smartphones was misleading. Each case is analyzed to determine how clinical decisions should be made.
The likelihood of donor site ischemia following the harvesting of a fibula flap is extremely low, but it is potentially lethal if it occurs. The authors describe a case of ischemia of the lower extremity following a free fibula harvest for head and neck reconstruction. The authors discuss preoperative, intraoperative, and postoperative strategies to assist in diagnosing and managing risks associated with free fibula flap harvesting in this paper.
This retrospective study on the keystone design perforator island flap (KDPIF) reconstruction offers valuable insights and compelling reasons for readers to engage with the article. By sharing clinical experience and reporting outcomes, the study provides evidence of the efficacy and safety profile of KDPIF as a reconstructive technique for soft tissue defects. The findings highlight the versatility, simplicity, and favorable outcomes associated with KDPIF, making it an essential read for plastic surgeons and researchers in the field. Surgeons worldwide have shown substantial interest in KDPIF, and this study contributes to the expanding knowledge base, reinforcing its clinical significance. Moreover, the study's comprehensive analysis of various parameters, including flap survival rate, complications, donor site morbidity, and scar assessment, enhances the understanding of the procedure's outcomes and potential benefits. The insights garnered from this research not only validate the widespread adoption of KDPIF but also provide valuable guidance for optimizing soft tissue reconstruction in diverse clinical scenarios. For readers seeking to explore innovative reconstructive techniques and improve patient outcomes, this article offers valuable knowledge and practical insights.
This comprehensive review article presents a profound exploration of critical facets within the realm of microsurgery, challenging existing paradigms. Through meticulous examination, the authors illuminate the intricate world of microangiosomes, dissection planes, and the clinical relevance of anatomical structures. Central to this discourse is an exhaustive comparative analysis of dermal plexus flaps, meticulously dissecting the viability and potential grafting applications of subdermal versus deep-dermal plexi. Augmenting this intellectual voyage are detailed illustrations, guiding readers through the intricate microanatomy underlying skin and adjacent tissues. This synthesis of knowledge not only redefines existing microsurgical principles but also opens new frontiers. By unearthing novel perspectives on microangiosomes and dissection planes and by offering a comparative insight into dermal plexus flaps, this work reshapes the landscape of microsurgery. These elucidations, coupled with visual aids, equip practitioners with invaluable insights for practical integration, promising to propel the field of microsurgery to unprecedented heights.
This article presents a groundbreaking surgical approach for treating facial paralysis, focusing on the combination of the pronator quadratus muscle (PQM) and the radial forearm flap (RFF). It addresses the challenges in restoring facial functions and skin closure in paralysis cases. The study's novelty lies in its detailed examination of the PQM's vascular anatomy when combined with the RFF, a topic previously unexplored. Through meticulous dissections, it provides crucial anatomical insights essential for enhancing facial reanimation surgeries, offering significant benefits in medical practices related to facial reconstruction and nerve transfer techniques.
This study introduces an advanced tubularized radial artery forearm flap (RAFF) technique, marking an enhancement over traditional methods in addressing complex nasal reconstructions. It integrates functional and aesthetic considerations through a structured, multi-stage reconstruction process, emphasizing the use of tubularized flaps. Key learning points include the detailed crafting of stable nasal passages, strategic use of costal cartilage for robust structural support, and tailored postoperative care with silicone splints. The tubularized RAFF technique not only optimizes patient outcomes and quality of life but also provides plastic surgeons with critical insights to refine their techniques in facial reconstruction. Indispensable for professionals in the field, this article enriches the understanding of sophisticated reconstructive challenges and solutions.
This article exemplifies a significant advancement in microsurgical techniques, highlighting the integration of robotic-assisted surgery into the deep inferior epigastric perforator (DIEP) flap procedure for breast reconstruction. It demonstrates how innovative robotic technology refines traditional methods, reducing the invasiveness of surgeries and potentially lessening postoperative complications like pain and herniation by minimizing the length of the fascial incision. This manuscript is pivotal for professionals in the medical field, especially those specializing in plastic surgery, as it provides a comprehensive overview of the operative techniques, benefits, and critical insights into successful implementation. Moreover, it underscores the importance of ongoing research and adaptation in surgical practices to enhance patient outcomes. The article serves as a must-read, not only for its immediate clinical implications but also for its role in setting the stage for future innovations in robotic-assisted microsurgery.
The groundbreaking study illuminates the complex mechanisms of nerve regeneration within fasciocutaneous flaps through meticulous neurohistological evaluation, setting a new benchmark in experimental microsurgery. It challenges existing paradigms by demonstrating the transformative potential of sensory neurorrhaphy in animal models, suggesting possible clinical applications. The data reveal a dynamic interplay of nerve recovery and degeneration, offering critical insights that could revolutionize trauma management and reconstructive techniques. By bridging experimental findings with hypothetical clinical scenarios, this article inspires continued innovation and research, aimed at enhancing the efficacy of flap surgeries in restoring function and sensation, thus profoundly impacting future therapeutic strategies.
This manuscript showcases an advanced surgical approach for treating malignant giant cell tumor of bone, emphasizing precision and ethical considerations. It leverages innovative pedicled flap technologies, as opposed to free flaps, enhancing limb functionality and patient quality of life. This technique equips surgeons with evidence that tailored surgical strategies can significantly improve outcomes in complex cases. The paper discusses technical challenges and highlights the application of supercharging and superdrainage techniques in limb reconstructions, methods well-established in microsurgery but infrequently used in oncological contexts. These techniques are crucial for optimizing flap viability and ensuring surgical success. Additionally, the manuscript underscores the profound impact of these advancements on patient lives, offering hope and showcasing tangible benefits. This narrative, blending scientific analysis with patient stories, enriches the understanding of limb reconstruction innovations in oncological surgery, making it invaluable for surgeons.
This systematic review and meta-analysis provide a pragmatic evaluation of drain-free versus drain-based DIEP flap techniques for breast reconstruction, challenging the traditional reliance on drainage. By analyzing postoperative outcomes, the study highlights the potential for refining surgical strategies to enhance patient comfort and recovery without compromising safety. The findings offer a neutral perspective, suggesting that clinical practice may not necessarily depend on the use of drains. This revelation prompts medical professionals to reassess existing surgical approaches and may catalyze a paradigm shift in postoperative care. Presented with clear narrative and rigorous data analysis, the article encourages readers to consider the broader implications of surgical innovations on patient care protocols.
This case highlights the use of a bipedicled deep inferior epigastric perforator (DIEP) flap for reconstructing a massive 45 × 17 cm chest wall defect following bilateral mastectomy. By preserving abdominal musculature and utilizing preoperative computed tomographic angiography (CTA) for perforator mapping, the technique enabled tension-free bilateral microvascular anastomosis to the internal mammary arteries. The incorporation of submuscular mesh and minimal donor-site undermining maintained abdominal wall integrity. At six-month follow-up, no hernia or functional deficits were observed, and the patient reported high satisfaction on the BREAST-Q. This muscle-sparing strategy offers a viable alternative for large, midline-crossing chest wall defects where conventional flaps may be insufficient.
Dr. Shyun-Jing Wee, the author of this article, met with the editors at SciTeMed as well as expert mentors to discuss the research in order to maximize its impact and ensure its wide dissemination. The webinar was moderated by Dr. Laura Chia-Fang Chen, a surgeon at Linkou Chang Gung Memorial Hospital who specializes in plastic and reconstructive surgery.
Dr. Peter Neligan and Dr. Isao Koshima were the guests of honor for this webinar. Both of them serve as Honorary Editors-in-Chief for International Microsurgery Journal.
Dr. Peter Neligan
Dr. Peter Neligan is a former president of the Plastic Surgery Foundation, of the American Society for Reconstructive Microsurgery, and of the North American Skull Base Society. He is also a former board member of the American Head & Neck Society. Previously, he served as a trustee of the American Society of Plastic Surgeons. He has authored more than 12 books, 85 book chapters, and over 200 peer-reviewed publications. At present, he serves as Editor-in-Chief of Plastic Surgery, a six-volume textbook used throughout the world for plastic surgery training. He has been invited to over 300 universities and major societies as a visiting professor or honored guest. In addition to sitting on several editorial boards, he has served as Editor-in-Chief of the Journal of Reconstructive Microsurgery in the past.
Dr. Isao Koushima

Dr. Isao Koushima, a former president of the World Society for Reconstructive Microsurgery, has made an enormous impact on the field of reconstructive microsurgery due to his leadership role. He is a former chairman of the Japanese Society for Surgery of the Hand, the Japanese Society of Reconstructive Microsurgery, and the Japanese Society for Lymphoreticular Tissue. In addition, he is the supervisor of the Japanese Society of Tissue Transplantation. He is also a member of the Japan Society for Head and Neck Surgery and the Japanese Research Society of Clinical Anatomy. In addition to his position as an emeritus professor at The University of Tokyo Hospital, he is also a distinguished professor at the Hiroshima University International Lymphedema Treatment Center.
Wee SJ, Lee JJ. Penopubic junction reconstruction using a pedicled superficial circumflex iliac artery perforator flap. Int Microsurg J 2022;6(1):5. https://doi.org/10.24983/scitemed.imj.2022.00164