Background: Effective nurse-led diabetes self-management education is essential for improving patient outcomes in acute care settings. This quality improvement project aimed to evaluate acute care nurses’ self-perceived competence and confidence in delivering diabetes education, identify barriers to effective teaching, and explore potential solutions.
Methods: A 12-question online survey was conducted from November 14 to 27, 2024, among 17 nurses in two acute care units of a tertiary hospital in British Columbia, Canada. The survey assessed self-rated competence in teaching and diabetes management, confidence in delivering education on specific topics, perceived barriers, and preferred learning formats. A targeted literature review using PubMed was performed to contextualize the findings.
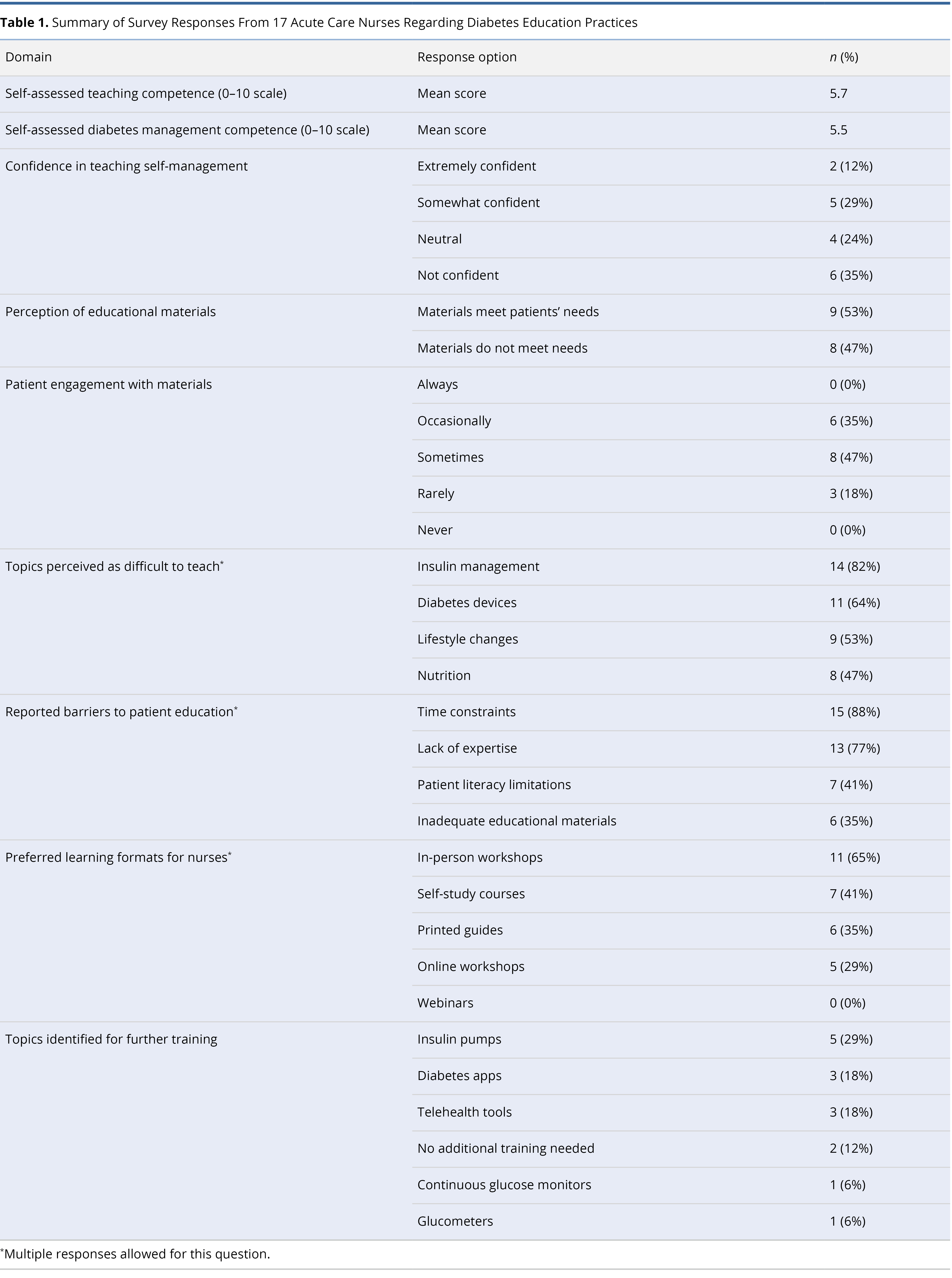
Results: Nurses reported moderate competence in teaching (mean 5.7/10) and diabetes management knowledge (mean 5.5/10), but low overall confidence, with only 12% feeling extremely confident in delivering education. Insulin management (82%), diabetes devices (64%), and lifestyle modification (53%) were identified as particularly challenging. Major barriers included time constraints (88%) and lack of expertise (77%). Preferred learning modalities were in-person workshops (65%) and self-directed study (41%). The literature review supported these findings, reflecting similar global trends in nurse confidence and competence.
Conclusion: This quality improvement initiative revealed substantial gaps in acute care nurses’ perceived competence and confidence in providing diabetes education, consistent with international evidence. Addressing these deficiencies requires the implementation of structured, targeted educational programs, investment in dedicated resources, and robust institutional support to enhance nursing capacity and improve diabetes care outcomes.
Diabetes is a chronic disease affecting millions worldwide [1] and remains a leading cause of morbidity and mortality [2]. According to the World Health Organization, approximately 14% of adults had diabetes in 2022, and its global prevalence is expected to rise significantly in the coming decades [1]. Effective management is essential to prevent complications, with patient education serving as a cornerstone of care [3]. Diabetes self-management education is consistently linked to improved glycemic control, enhanced quality of life, and reduced complication rates [3,4]. Beyond individual benefits, it also helps reduce the overall burden on healthcare systems [5].
To be effective, educational interventions must be tailored to each patient's needs, considering factors such as health literacy, cultural context, and preferred learning styles [6]. Despite its critical role, diabetes education delivery faces persistent barriers, especially in acute care settings where nurses are key educators. A recent quality improvement initiative in Quebec identified major obstacles, including fragmented care integration, poor interprofessional collaboration stemming from unclear role definitions, and a lack of standardized, evidence-based training for healthcare professionals [7].
Building on these insights, the current quality improvement project evaluates diabetes education practices among acute care nurses in British Columbia, Canada. It examines nurses’ self-perceived competence and confidence in delivering diabetes education, identifies key barriers to effective teaching, and explores evidence-based strategies to enhance educational delivery in this setting.
A nursing needs assessment was conducted between the 14th and 27th of November, 2024, at a tertiary acute care hospital in British Columbia, Canada. Data were collected using a self-developed, 12-item online survey administered via Microsoft Forms (see Supplementary Table S1). The survey targeted nurses from units with the highest frequency of Diabetes Nurse Educator referrals and aimed to evaluate their confidence in delivering diabetes education, identify preferred learning formats, explore perceived barriers to effective teaching, and determine the resources needed to enhance patient self-management education.
To facilitate participation, a Quick Response (QR) code linking to the survey was distributed by the hospital’s Diabetes Nurse Educator across the relevant nursing units. Participation was voluntary and anonymous. As this initiative was classified as a standard practice review and internal quality improvement project, formal ethics approval was not required. In accordance with institutional guidelines for such activities, informed consent was implied through voluntary completion of the survey.
To contextualize the findings and assess whether they reflected local practice conditions or broader systemic challenges, a targeted literature review was conducted. The findings of this review are detailed in Supplementary File S1 (Supplementary Materials: Literature Review).
A total of 17 nurses completed the online survey, representing two acute care units: one medical and one cardiac specialty. The average time required to complete the 12-item questionnaire was 10 minutes and 46 seconds. This duration included responses to both closed-ended questions and one open-ended item designed to capture additional qualitative insights. A summary of the key findings is presented in Table 1.

Level of Competence
Nurses were asked to assess their competence in two primary domains. The first focused on teaching skills, including the ability to instruct patients on symptom management, medication adherence, physician notification, and blood glucose monitoring. The second assessed their knowledge of diabetes management, encompassing pharmacological properties and side effects of glucose-lowering agents, insulin pharmacodynamics, management of hypo- and hyperglycemia, and strategies for lifestyle modification.
Using a 0-to-10 rating scale, participants reported an average score of 5.7 for teaching skills and 5.5 for diabetes management knowledge. These results indicate a moderate level of self-perceived competence in both areas.
Level of Confidence in Delivering Diabetes Education
Overall, nurses reported low levels of confidence in providing diabetes education. Only 12% indicated that they felt extremely confident in teaching key aspects of diabetes management, while 59% expressed either neutrality or a lack of confidence.
The area most frequently identified as challenging was insulin management, reported by 82% of respondents. Other difficult topics included diabetes device use (64%), lifestyle modification (53%), and nutritional counseling (47%).
Challenges and Barriers
Several barriers to effective diabetes education were identified. Time constraints emerged as the most significant, with 88% of nurses citing limited time as a major impediment. Additionally, 77% reported a lack of expertise, 41% noted challenges related to patient literacy, and 35% pointed to insufficient educational materials.
Nearly half of the respondents (47%) believed that current teaching materials did not adequately meet patients’ educational needs. An equal proportion indicated that patients only sometimes understood the information provided. Notably, no nurse felt that patients were consistently engaged with the education they received.
Preferred Learning Formats
When asked about preferred formats for further education in diabetes management, 65% of nurses selected in-person workshops. This was followed by self-study courses (41%), printed guides (35%), and online workshops (29%). Notably, none of the respondents found webinars useful, indicating a general preference for more interactive or hands-on learning modalities.
Topics of Importance
Respondents identified several priority areas where additional training was needed. The most frequently cited topics were insulin pump education (29%), mobile diabetes applications such as MySugr and MyFitnessPal (18%), and telehealth technologies, including cloud-based monitoring platforms and remote patient monitoring systems (18%).
Nursing Voice
All participants contributed free-text responses, offering deeper insights into the challenges of delivering diabetes education in inpatient settings. Common themes included chronic staffing shortages, the increasing complexity of diabetes-related technologies, and the absence of specialized educators.
One nurse commented, “We already spend approximately one hour teaching and preparing discharges... and we are short-staffed with no ability to add more tasks.” Another emphasized the importance of a designated educator, stating, “Having a diabetes education nurse specifically trained to provide diabetic patient teaching is critical... It would be safer to have someone who specializes in this type of teaching.” Others voiced concern about the rapid pace of technological advancement, with one noting, “There are so many new devices that did not exist when I went through school – I am not familiar at all with pumps or continuous monitoring.”
This survey highlights notable gaps in both competence and confidence among acute care nurses in delivering diabetes education. While respondents demonstrated a foundational understanding of diabetes care, their moderate self-assessments in teaching skills and overall knowledge reveal substantial room for improvement. Insulin management and the use of diabetes-related devices were particularly challenging, indicating an urgent need for targeted educational support in these areas.
The most frequently reported barriers included time constraints, limited expertise, and patient literacy challenges. These findings reflect the structural and contextual complexities that impede effective patient education in acute care settings. Addressing these challenges will require structured interventions, such as protected time for education, competency-based training programs, and the development of accessible, patient-centered teaching materials.
Nurses expressed a strong preference for interactive and practical learning formats, particularly in-person workshops. This preference underscores the value of practice-oriented environments that can enhance both confidence and knowledge retention. At the same time, the rapid integration of technology into diabetes care, including insulin pumps, mobile applications, and telehealth platforms, requires ongoing professional development to ensure that nurses remain proficient with these evolving tools.
The results also highlight the pressing need for dedicated diabetes educators within inpatient settings. Many respondents reported feeling underprepared to address complex care needs and technological advancements without specialized support. Integrating diabetes educators into the clinical team may help bridge these gaps, facilitate consistent and up-to-date education for patients, and better support nurses in their instructional roles.
Overall, these findings underscore the importance of institutional investment in nursing professional development. Strengthening nurses’ knowledge, skills, and access to resources is essential for improving the quality and consistency of diabetes self-management education, ultimately contributing to better patient outcomes in acute care environments.
Confidence in Diabetes Education
Our survey revealed that nurses generally reported low confidence in delivering diabetes education, with insulin management identified as particularly challenging. This finding is consistent with international literature. Studies from New Zealand, Iran, and Saudi Arabia similarly documented persistent gaps in nurse confidence, with many nurses feeling inadequately prepared to provide effective diabetes care [8–10]. In Australia, Holton et al. observed that nurses and midwives working in public health settings often felt underconfident due to insufficient educational preparation [11]. In China, Hu and Jiang found that although 96% of participants demonstrated strong competence in glucose monitoring, nearly half (49%) lacked confidence in recognizing the signs of hypo- and hyperglycaemia [12]. By contrast, a Danish study reported relatively high confidence levels among 101 hospital-based nurses, with mean scores of 8.4/10 for diabetes management and 8.0/10 for continuous glucose monitoring. These findings suggest that institutional context may significantly influence perceived competence [13].
A cross-sectional survey of 160 nurses working at two teaching hospitals in Iran revealed a significant relationship between the hospital of employment and nurses' competence in diabetic nutritional management. This relationship was observed in both perceived competence and actual clinical performance. Perceived competence was defined as confidence in clinical practice. Nurses at the second hospital reported higher practice scores. The authors suggested that this difference may reflect varying levels of exposure to patients with diabetes between the two institutions [9]. These findings suggest that the work environment may influence both confidence and competence. However, it remains unclear whether this is due to increased clinical experience, higher quality training, stronger institutional support, better access to resources, or other contextual factors. Importantly, confidence does not always correspond to actual competence. A cross-sectional survey of 325 nurses in Saudi Arabia found that some individuals with high perceived knowledge scores demonstrated significantly lower actual knowledge of diabetes. Notably, this group included nurses who had participated in diabetes workshops and courses. This raises concerns about the effectiveness, content, or knowledge retention associated with such educational interventions [10].
Although some studies have reported increased confidence among nurses in specific clinical settings or following additional training [11,13], the broader trend remains consistent with our findings. Many nurses continue to face persistent challenges in developing and maintaining confidence. These difficulties are particularly evident when managing emerging technologies in diabetes care and navigating the increasing complexity of patient needs. Our project identified substantial gaps in insulin-related education. In response, several interventions have been proposed. One approach involves the use of insulin pump toolkits. These toolkits are intended to support nurse training, improve knowledge, and strengthen both clinical confidence and patient trust [14]. Another study highlighted the importance of addressing psychological distress related to diabetes. It emphasized the need for practical strategies to help nurses respond to this challenge. The study also underscored the value of structured training and professional supervision in enhancing nurses’ ability to provide effective education [15].
Competence in Diabetes Education
Our survey revealed moderate self-assessments in both teaching skills and diabetes management knowledge. The average scores were 5.7 out of 10 for teaching and 5.5 out of 10 for knowledge. Participants also reported substantial gaps in specific areas, including insulin management, the use of diabetes-related devices, and strategies for lifestyle modification. Similar competency gaps have been documented in other studies. In China, a survey of 4,011 nurses found that while 74% demonstrated general knowledge of diabetes, only 34% were considered competent in pharmacological management [12]. An integrative review by Alotaibi identified widespread knowledge deficits across international studies. These deficits were particularly evident in areas such as oral hypoglycaemic agents, insulin therapy, blood glucose monitoring, and nutritional management [16]. In the United States, nurses similarly reported a limited understanding of diabetes care, especially in relation to insulin pump use [14].
Even when nurses possess sufficient knowledge, gaps in practical competence may still persist. For example, a study from South Africa reported that 84.8% of nurses demonstrated moderate-to-good knowledge of diabetic foot care. However, more than half were unaware of available screening tools and required additional training [17]. Another study conducted in South African primary care settings found that 75% of nurses exhibited high overall knowledge. Despite this, knowledge gaps remained in specific areas. Only 45% of participants correctly identified the causes of hyperglycaemia [18]. In that study, nurses achieved high scores in both knowledge, with a mean of 11.9 out of 14, and in self-efficacy. These results suggest that postgraduate education and hands-on clinical experience may contribute to improved competence [18]. This observation is further supported by findings from Duprez et al. In a sample of 472 nurses and 51 nursing students, those with advanced degrees demonstrated greater effectiveness in diabetes self-management support compared to less educated or less experienced counterparts [19].
Daly et al. compared diabetes management competence between two cohorts of primary healthcare nurses in New Zealand. One cohort was from 2006 to 2008, and the other from 2016. The study observed improvements over time [8]. In the 2016 cohort, more nurses pursued postgraduate education, consulted clinical guidelines, and addressed various aspects of diabetes care with patients. These aspects included discussing laboratory results and providing advice on lifestyle modifications. However, fewer than 20% of nurses in the 2016 cohort recognized smoking, hypertension, and dyslipidemia as risk factors for diabetic complications. Only 37% felt they had sufficient knowledge to provide guidance related to medications [8]. Researchers in Australia have similarly reported that nurses often struggle to keep pace with the rapid evolution of diabetes medications [11]. As medical innovations continue to advance, particularly in pharmacotherapy and digital health technologies, healthcare professionals increasingly find it difficult to stay current with new developments [11,20]. Taken together, these findings suggest that although competency levels vary depending on context, many nurses continue to face challenges similar to those identified in our survey. Regular, targeted diabetes education and reliable access to experienced clinical mentors have been shown to improve nurses’ knowledge. These efforts also enhance their ability to counsel patients on medications, lifestyle changes, and other essential components of diabetes care [8,11,16–18].
Challenges in Nurse Instruction
The rapid pace of change in diabetes care, combined with ongoing resource limitations, makes it challenging for nurses to remain current with evolving therapies and technologies [11,21]. This concern was echoed by respondents in our survey. Time constraints emerged as the most significant barrier, with 88% of participants identifying limited time as a major obstacle. Other frequently reported challenges included a lack of expertise, patient literacy difficulties, and the inadequacy of available educational materials.
These findings are consistent with prior research. Studies have documented numerous barriers to effective education delivery, including high workloads, limited resources, increasing patient acuity, complex medication regimens, time pressure, insufficient supervision, and environmental distractions such as noise and lack of privacy [11,16,18,22].
In the United States, nurses have reported difficulty in trusting patients to manage their insulin pumps independently. These concerns often relate to patient safety and limited patient knowledge or capacity [14]. Broader systemic barriers, such as nursing shortages and financial constraints, further exacerbate these difficulties [16]. Structural issues also persist across healthcare settings. These include restrictive role definitions, excessive workloads, and inadequate academic or clinical training [11,16,18].
Importantly, these challenges are not limited to nurses. Diabetes educators face similar obstacles. A qualitative study from Iran found that although educators were knowledgeable about diabetes content, many lacked formal training in educational methods. Their teaching relied primarily on personal experience and immediate patient needs rather than on structured instructional strategies tailored to the learning preferences of nurses [22].
Many of these educators had received training more than ten years ago, with some reporting as little as four hours of total instruction. Continuing education opportunities were described as infrequent, inaccessible, or unavailable. Several participants reported that updated, evidence-based resources were difficult to find. When available, such resources were often only published in English or hidden behind paywalls costing between 30 and 70 US dollars, which many found unaffordable [22].
Improving the training of diabetes educators is essential. Without adequate preparation, educators are unable to support the development of nursing knowledge or facilitate effective patient self-management. The barriers identified in our study, particularly time constraints, limited expertise, and poor access to educational resources, are widely documented in the literature. These findings emphasize that diabetes education remains a global challenge that requires coordinated reform across structural, institutional, and educational domains [11,16,18].
Fixing Gaps in Diabetes Teaching
Aloitabi’s 2016 systematic integrative review provides a comprehensive, global perspective on diabetes education for nurses by synthesizing data from multiple countries [15]. One of the review’s key strengths lies in its identification of recurring knowledge deficits and systemic patterns across diverse healthcare systems. These findings offer valuable insights for policymakers and educators involved in the design of international training initiatives.
For instance, the review notes that in Britain, nurses' limited knowledge of diabetes and its management is associated with low participation in continuing education programs [15]. This suggests that effective strategies must address not only educational content but also the underlying causes of nonparticipation.
In many developing countries, limited access to resources and financial barriers restrict nurses’ ability to participate in external diabetes training programs. Strategies aimed at improving nursing knowledge and skills in these contexts must therefore focus on enhancing both the availability of resources and the accessibility of educational opportunities [15].
The review also highlights structural challenges, including inconsistent clinical guidelines and varying levels of professional education and development, which continue to hinder effective nursing practice on a global scale [15].
While the current study identifies specific and immediate barriers experienced by nurses, Aloitabi’s findings underscore a broader systemic issue. Many nurses worldwide begin their professional careers without sufficient training in diabetes management [15]. These deficiencies are not merely individual shortcomings; rather, they are deeply embedded within nursing education curricula and the continuing professional development infrastructure.
Facilitators and Effective Strategies
Participants in our survey expressed a clear preference for in-person workshops, self-directed learning modules, and printed guides, while demonstrating limited enthusiasm for online workshops. Specific training needs were identified in areas such as insulin pump education, mobile diabetes applications, and telehealth technologies. Respondents also emphasized the critical importance of specialized diabetes educators in supporting nursing practice. Similarly, Holton et al. highlighted the value of ongoing education and the integration of dedicated diabetes resource personnel to address persistent knowledge gaps among nursing staff [12].
Multiple studies have demonstrated that postgraduate education, continuous professional development, and mentorship from experienced practitioners significantly enhance nurses’ knowledge and clinical performance [10,12,16,18,19]. A systematic review and meta-analysis further supported the effectiveness of technology-enhanced diabetes education programs. These included mobile applications, high-fidelity simulation, and virtual learning environments, all of which contributed to improved knowledge, skill performance, self-confidence, and learner satisfaction among nursing students [23]. However, the analysis did not reveal a statistically significant advantage of technology-based interventions over traditional educational methods [23].
The literature consistently underscores the importance of structured educational programs. Core components include roleplaying, professional supervision, multidisciplinary meetings, collaborative diabetes education teams, and the use of customized teaching materials [8,9,12–17]. In parallel, diabetes educators must have access to ongoing professional development, accredited scientific literature, and expert-led training in instructional methodology. Effective diabetes education requires not only clinical expertise in disease management but also advanced proficiency in educational delivery strategies [22].
Several tools and resources have been proposed to bridge the gap between perceived and actual competence. These include evidence-based clinical guidelines, practical toolkits, standardized checklists, and digital resources such as interactive modules, instructional videos, and telehealth platforms [10,11,14,15,17]. All nurses, regardless of experience level, should engage in regular continuing education. Recommended strategies include quarterly multidisciplinary sessions focused on updated clinical guidelines and emerging therapies, annual in-service seminars, and freely accessible online modules that support flexible, needs-based learning [16].
Recommendations
In Canada, the growing reliance on foreign-trained nurses due to an ongoing nursing shortage underscores the urgent need for standardized diabetes education across the nursing workforce. As Albagawi noted, variations in the quality of nursing education across countries may contribute to disparities in clinical knowledge and the delivery of diabetes care [10]. It is therefore critical that all nurses, regardless of their country of training, have access to current clinical guidelines to ensure consistent and evidence-based care. However, Canadian-trained nurses are not inherently more knowledgeable or better prepared. As reported by Alotaibi et al., knowledge gaps in diabetes management persist across both developed and developing nations [16]. The central objective should be to ensure that all nurses in British Columbia receive standardized, high-quality training and operate under uniform evidence-based guidelines, irrespective of their educational background.
To address persistent deficiencies in diabetes education, we propose a multifaceted strategy that integrates local needs with global evidence. A critical first step is the development of targeted curriculum modules specifically designed for acute care settings. These modules should emphasize core competencies such as insulin management, education on insulin pumps and continuous glucose monitors, lifestyle counseling, and digital health literacy. Educational content should be interactive, case-based, and competency-driven, tailored to clinical scenarios encountered in inpatient care. Postgraduate education and continuing professional development have been shown to significantly enhance nurses’ knowledge and confidence in diabetes management [12,18,19]. Including frontline nurses, certified diabetes educators, and academic stakeholders in curriculum development will ensure clinical relevance and feasibility.
Equally important is the establishment of a province-wide professional development framework that includes protected time for continuing education. Policy and financial support from health authorities is essential to allow nurses to participate in diabetes training without compromising their clinical responsibilities. Making diabetes education a formal component of annual professional competency reviews could further promote accountability and engagement.
Interdisciplinary collaboration should also be prioritized through structured, team-based learning. Nurses should have access to specialized diabetes educators, clinical champions, and regular interprofessional case discussions. These collaborative practices foster role clarity and shared responsibility in diabetes care, as highlighted in prior research [8,10,11,13,16].
Educational delivery must be flexible and accessible. In-person workshops should be supplemented with digital tools and self-directed learning opportunities. Training should include hands-on use of mobile applications, telehealth systems, and cloud-based monitoring tools, which are increasingly integral to modern diabetes management [21]. A multimodal delivery approach—combining printed guides, online modules, and simulation-based learning—can accommodate diverse learning preferences and scheduling constraints.
Finally, we recommend the creation of a centralized, publicly accessible provincial platform for diabetes education resources. This repository should include evidence-based materials aligned with provincial standards and be available in multiple languages. Developing culturally tailored content in collaboration with patient partners will further enhance relevance and usability. Ensuring that nurses have access to consistent, high-quality educational materials will help reduce variability in practice and support the delivery of patient-centered care.
By adopting this comprehensive strategy, healthcare leaders and educators in British Columbia can build a sustainable and equitable infrastructure for diabetes education. These efforts will improve nursing competence and confidence, promote consistency in care delivery, and ultimately enhance outcomes for individuals living with diabetes.
Unique Contribution to Acute Care
This quality improvement project makes a distinct contribution to the field of acute care by highlighting the systemic and educational challenges frontline nurses face when delivering diabetes education in high-pressure hospital environments. Unlike community or outpatient settings, acute care is defined by unique operational constraints, including brief patient stays, high turnover, frequent interruptions, and limited opportunities for meaningful patient engagement. These factors significantly impede the delivery of effective bedside education and knowledge transfer. This project offers a preliminary exploration of these challenges, shedding light not only on the local state of nursing competence and confidence, but also on broader environmental and institutional barriers that undermine the quality of diabetes education in hospital-based care.
A key contribution of this work lies in translating nurse-identified barriers into feasible, context-specific strategies tailored for acute care. Recommendations include the implementation of structured in-service education programs, utilization of point-of-care teaching tools, and integration of certified diabetes educators within hospital units to support overextended clinical teams. The project also underscores the importance of protected time for education, streamlined access to digital teaching materials, and interdisciplinary care models that frame diabetes education as a collective responsibility across the healthcare team.
The findings further emphasize the need to implement scalable, competency-based educational frameworks adaptable to nurses with varying levels of experience and educational preparation. This is particularly relevant within the Canadian healthcare context, where acute care units are increasingly staffed by internationally educated nurses and recent graduates who may lack exposure to local diabetes guidelines or technologies. To address this gap, the project proposes standardized, modular education programs supported by quick-reference materials, mobile-accessible content, and structured mentorship provided by certified diabetes educators. Such measures offer a pragmatic approach to building workforce capacity in alignment with the operational demands of hospital care.
Moreover, the study reinforces the critical role acute care nurses play in transitional care, particularly in preventing readmissions and ensuring safe discharge for patients with diabetes. Strengthening the educational capacity of nurses in this setting has the potential to directly impact system-level outcomes, including shorter hospital stays, fewer complications, and improved patient self-management post-discharge.
Finally, this project advocates for a cultural shift in acute care, positioning diabetes education as a core nursing competency rather than an ancillary task. Institutional leadership, policy initiatives, and clinical infrastructure must support this transformation by embedding patient education into standard workflows and performance expectations.
In summary, this quality improvement initiative moves beyond identifying educational deficits. It provides a focused, practical, and contextually grounded strategy for strengthening diabetes education in acute care settings, with clear implications for professional development, patient safety, and care continuity.
Limitations and Contextual Considerations
This project, like many international studies in the field, relied on self-assessment tools. While such instruments are valuable for evaluating perceived competence, they may not accurately reflect actual knowledge or clinical skill. Discrepancies between self-perceived and objectively demonstrated competence have been well documented, underscoring the need for complementary assessment methods capable of revealing true knowledge gaps and informing targeted educational interventions [9,10].
The survey employed in this project was self-developed and lacked formal psychometric validation, which may affect the reliability and generalizability of the findings. Additionally, the small sample size and restriction to acute care units within a single institution further limit the applicability of results to broader populations. However, in keeping with the exploratory and pragmatic aims of quality improvement, this study prioritized the generation of context-specific insights over statistical generalizability.
Descriptive statistics were used to summarize the data and identify salient trends in self-reported competence and confidence. The primary objective was to guide practical improvements in local practice rather than to establish causal inferences or produce population-wide estimates. Despite these methodological constraints, the recurring themes identified across diverse international studies suggest that the challenges uncovered in our project are not isolated. Nurses in various healthcare systems continue to encounter similar barriers to delivering effective diabetes education, reinforcing the global imperative for sustained professional development in this area.
Future initiatives should consider adopting a multi-site or regionally coordinated approach using a psychometrically validated instrument and a larger, randomly selected sample. Such a design would enable a more comprehensive assessment of diabetes education practices among nurses across British Columbia and support the development of standardized, scalable educational interventions.
This quality improvement project identifies persistent challenges in delivering diabetes self-management education in acute care. Nurses demonstrated moderate competence but reported low confidence, particularly with new technologies. Time constraints, limited expertise, and inadequate resources further hinder effective education. These challenges reflect global trends and reveal systemic gaps in nursing education. Addressing them requires structured, competency-based training, interdisciplinary collaboration, and institutional support. Future initiatives should evaluate the long-term effects of educational interventions on nursing performance and patient outcomes. Improving these areas is essential for advancing the quality and consistency of diabetes care.
Received date: April 02, 2025
Accepted date: June 11, 2025
Published date: August 01, 2025
We sincerely thank Fraser Health for their generous funding of this project and for their valuable support throughout the preparation of this manuscript.
The manuscript has not been presented or discussed at any scientific meetings, conferences, or seminars related to the topic of the research.
The study adheres to the ethical principles outlined in the 1964 Helsinki Declaration and its subsequent revisions, or other equivalent ethical standards that may be applicable. These ethical standards govern the use of human subjects in research and ensure that the study is conducted in an ethical and responsible manner. The researchers have taken extensive care to ensure that the study complies with all ethical standards and guidelines to protect the well-being and privacy of the participants.
Authors CK and AL received funding from Fraser Health to support the preparation of this manuscript. Authors BK, SF, LR, and KK are employed by Fraser Health.
In accordance with the ethical standards set forth by the SciTeMed publishing group for the publication of high-quality scientific research, the author(s) of this article declare that there are no financial or other conflicts of interest that could potentially impact the integrity of the research presented. Additionally, the author(s) affirm that this work is solely the intellectual property of the author(s), and no other individuals or entities have substantially contributed to its content or findings.
It is imperative to acknowledge that the opinions and statements articulated in this article are the exclusive responsibility of the author(s), and do not necessarily reflect the views or opinions of their affiliated institutions, the publishing house, editors, or other reviewers. Furthermore, the publisher does not endorse or guarantee the accuracy of any statements made by the manufacturer(s) or author(s). These disclaimers emphasize the importance of respecting the author(s)' autonomy and the ability to express their own opinions regarding the subject matter, as well as those readers should exercise their own discretion in understanding the information provided. The position of the author(s) as well as their level of expertise in the subject area must be discerned, while also exercising critical thinking skills to arrive at an independent conclusion. As such, it is essential to approach the information in this article with an open mind and a discerning outlook
2025 The Author(s). The article presented here is openly accessible under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). This license grants the right for the material to be used, distributed, and reproduced in any way by anyone, provided that the original author(s), copyright holder(s), and the journal of publication are properly credited and cited as the source of the material. We follow accepted academic practices to ensure that proper credit is given to the original author(s) and the copyright holder(s), and that the original publication in this journal is cited accurately. Any use, distribution, or reproduction of the material must be consistent with the terms and conditions of the CC-BY license, and must not be compiled, distributed, or reproduced in a manner that is inconsistent with these terms and conditions. We encourage the use and dissemination of this material in a manner that respects and acknowledges the intellectual property rights of the original author(s) and copyright holder(s), and the importance of proper citation and attribution in academic publishing.
Appendix 1. Supplementary Table S1. Full List of Survey Questions
Appendix 2. Supplementary File S1. Supplementary Materials
The authors investigate nurses’ self-perceived competence and confidence in delivering diabetes education, offering insights into barriers and training needs within acute care settings. This work has the potential to inform targeted educational interventions and enhance the quality of diabetes care. However, the manuscript contains critical flaws that undermine its suitability for publication. The small sample size (17 nurses) limits the generalizability of the findings, and the use of an unvalidated survey tool raises concerns about data reliability. In addition, the literature review is constrained by narrow search criteria, which compromises its comprehensiveness. These issues, including the limited sample size, lack of instrument validation, and incomplete literature synthesis, significantly weaken the study’s rigor and overall impact. Unless these concerns are addressed through substantial revision, the manuscript does not meet the standards required for publication in its current form.
A TRL was conducted because it offers a pragmatic, efficient, and sufficiently rigorous approach to support the objectives of this quality improvement projects. Systematic reviews, while valuable, are more resource-intensive and time consuming, which is why we opted for a TRL to deliver timely, focused insights.
A targeted review aims to synthesize the most pertinent and actionable evidence rather than exhaustively catalogue all historical studies. A TLR can be conducted in weeks, and enables timely, focused synthesis of the most relevant literature to inform practice and policy, making it the preferred choice for this context. TLRs are widely used and accepted in healthcare research, especially for projects where the research question is focused and resources are limited. We have now justified the use of a TLR rather than a SLR in the manuscript under the Supplementary Materials: Literature Review document.
To address the reviewer's concern, we have now expanded our search scope. Specifically, we included the Cochrane and CINAHL databases in addition to PubMed, lifted the English-language restriction, and extended the search to cover the last 10 years. We also updated the manuscript (Supplementary Materials: Literature Review) to reflect these changes, including the PRISMA flow diagram (Supplementary Figure S1) and Table 2 (Supplementary Materials: Literature Review).
Furthermore, we acknowledge the exclusion of paywalled articles was intentional to avoid potential access barriers. However, we also performed a re-check of the search without the English-language restriction, which identified a few additional studies in other languages (Chinese, French, and Spanish), which were noted but not included in the manuscript due to their limited relevance to our focus (Supplementary Materials: Literature Review).
The decision to limit the search to the past 5 years was made to capture the most up-to-date evidence, given the rapidly evolving healthcare environment, especially in light of the COVID-19 pandemic and its impact on healthcare systems. We have updated the Supplementary Materials: Literature Review document to include the expanded search parameters and discussed the limitations of our approach in the context of language and publication biases in the Limitations and Contextual Considerations section (Supplementary Materials: Literature Review). Based on the new search results, we have updated the manuscript discussion (page 10, 12, 13).
On the other hand, we have considered other strategies and have expanded our search to include the CINAHL database, and we have rerun the search in PubMed, as noted above. The time limit in both databases was expanded to 10 years, and there was no language restriction. The revised literature review now incorporates additional studies, and we have updated the PRISMA flow diagram (Supplementary Figure S1), Table 1 (Supplementary Materials: Literature Review) accordingly. We also discuss the limitations of our original approach and the potential for language and publication bias in the revised manuscript (Supplementary Materials: Literature Review). The discussion section of the main manuscript has been revised to include the new search results (page 10, 12, 13).
I commend the authors for addressing nurses’ self-perceived competence in diabetes education within acute care. This is a vital issue given the rising prevalence of diabetes and the critical role nurses play in supporting patient self-management. The findings, such as moderate perceived competence, low confidence, and reported barriers including time constraints and limited expertise, reveal significant gaps in nursing education and suggest important opportunities for improvement. The study’s originality lies in its focus on acute care settings and its integration of global literature to contextualize local challenges. By building upon earlier studies, the authors aim to contribute more in-depth insights, particularly regarding training needs for technologies such as insulin pumps.
Nonetheless, several key limitations remain. The absence of inferential statistical analysis or qualitative methodology limits the ability to explore relationships between variables. Furthermore, the discussion section does not clearly highlight the study’s unique contributions in the context of acute care. The recommendations also remain general and would benefit from greater specificity. To enhance both the academic and practical impact of this work, further attention to the following areas is recommended:
Koning C, Lock A, Kelly B, Finamore S, Rosenzweig L, Kainth K. Assessment of nurses’ self-perceived competence and confidence in providing diabetes education: A quality improvement initiative. Diabetes Endocrinol 2025;3(1):1. https://doi.org/10.24983/scitemed.de.2025.00199