Objective: Button battery ingestion poses a significant risk of morbidity and mortality in the pediatric population following esophageal impaction. The Area Deprivation Index (ADI) reflects a geographic area's level of socioeconomic deprivation based on household income, employment status, education level, and housing quality. This study aimed to evaluate the associations between elevated ADI and button battery ingestion.
Methods: Through a 12-year retrospective single-center study of patients under age 14 with suspected foreign body ingestion, 1,017 subjects were identified using ICD 9 and 10 codes for airway and esophageal foreign body ingestion, of which 324 met the inclusion criteria. ADI was calculated using the patient's address, with "high" being greater than the 50th percentile. We employed binary multivariable logistic regression to predict high illness severity.
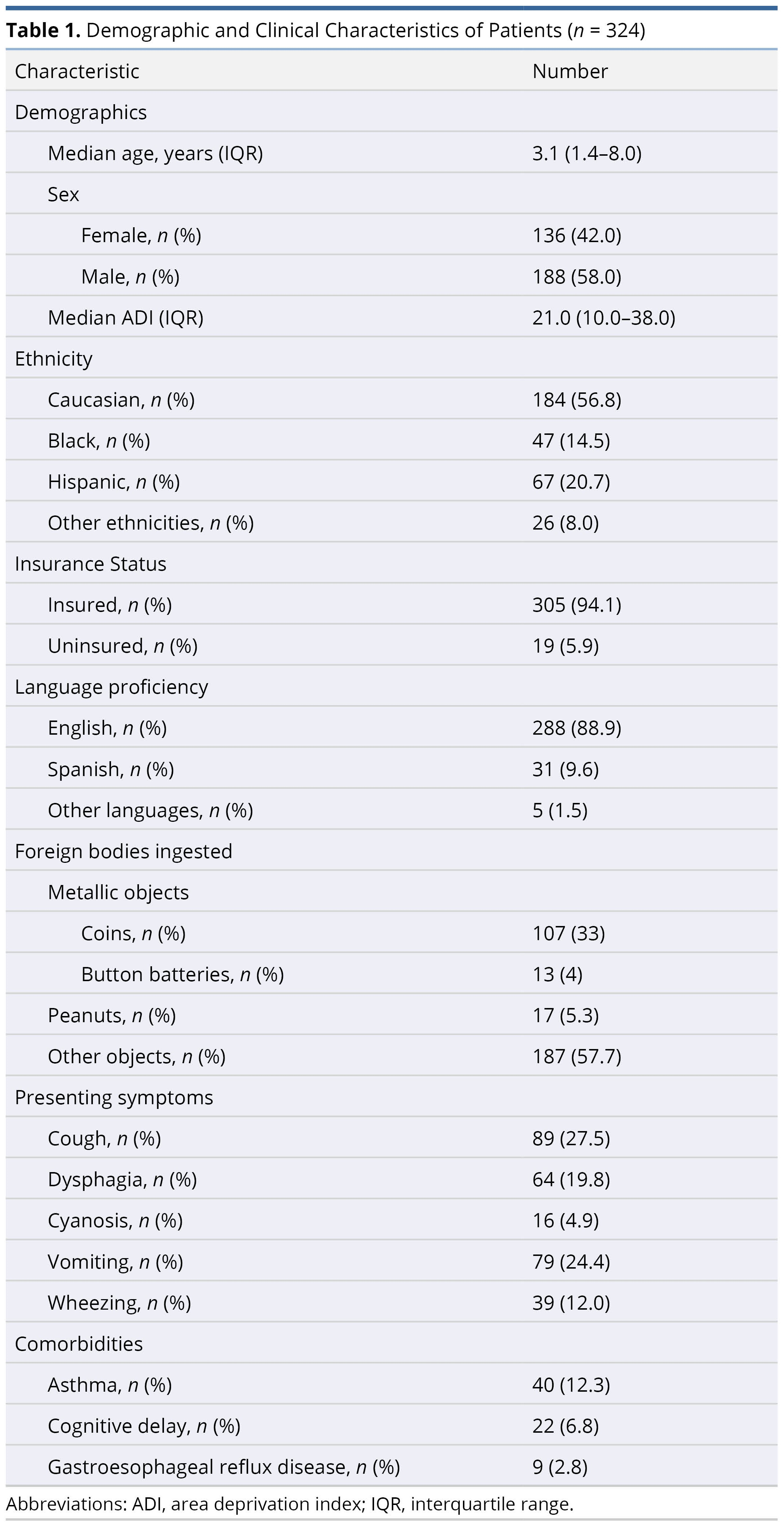
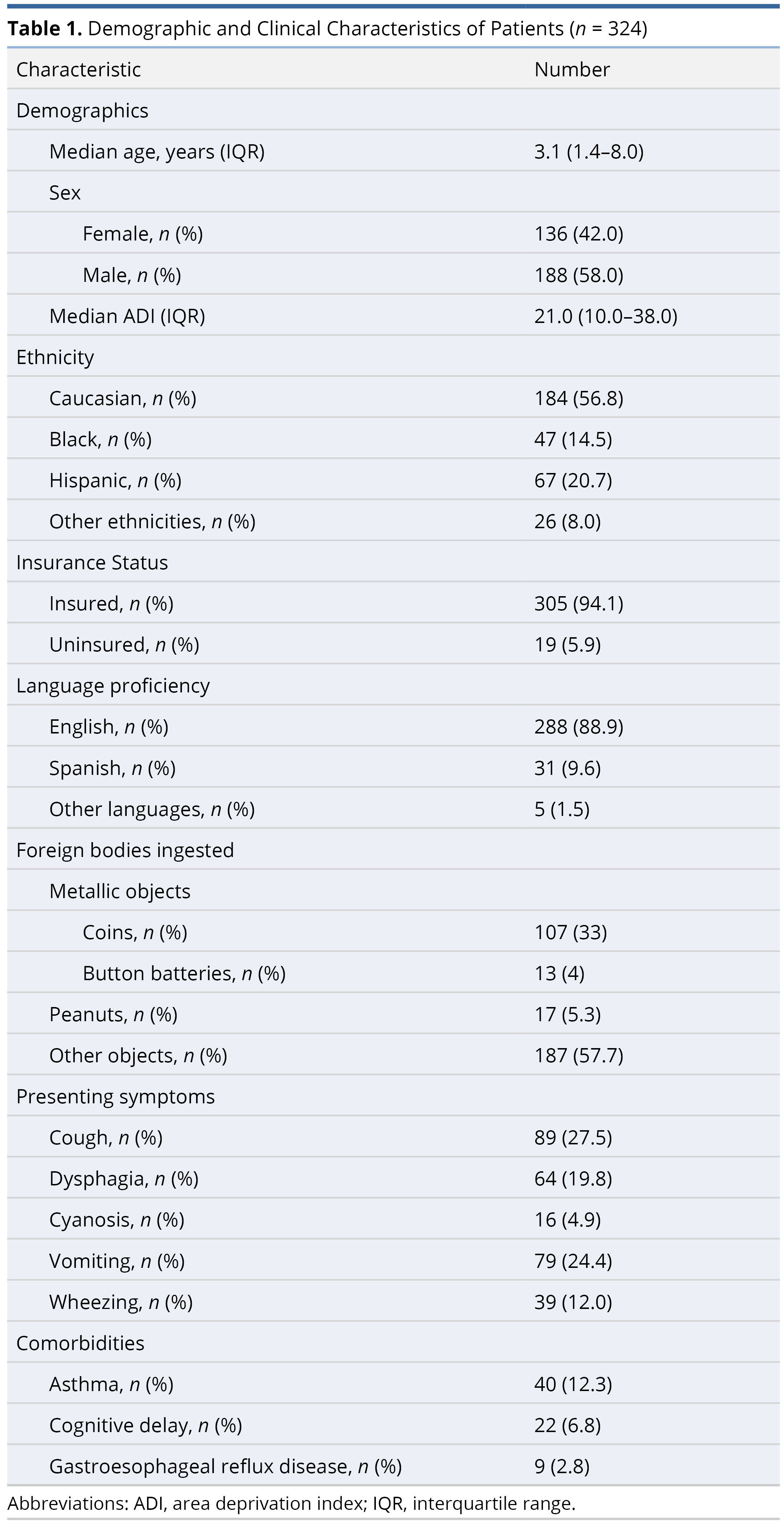
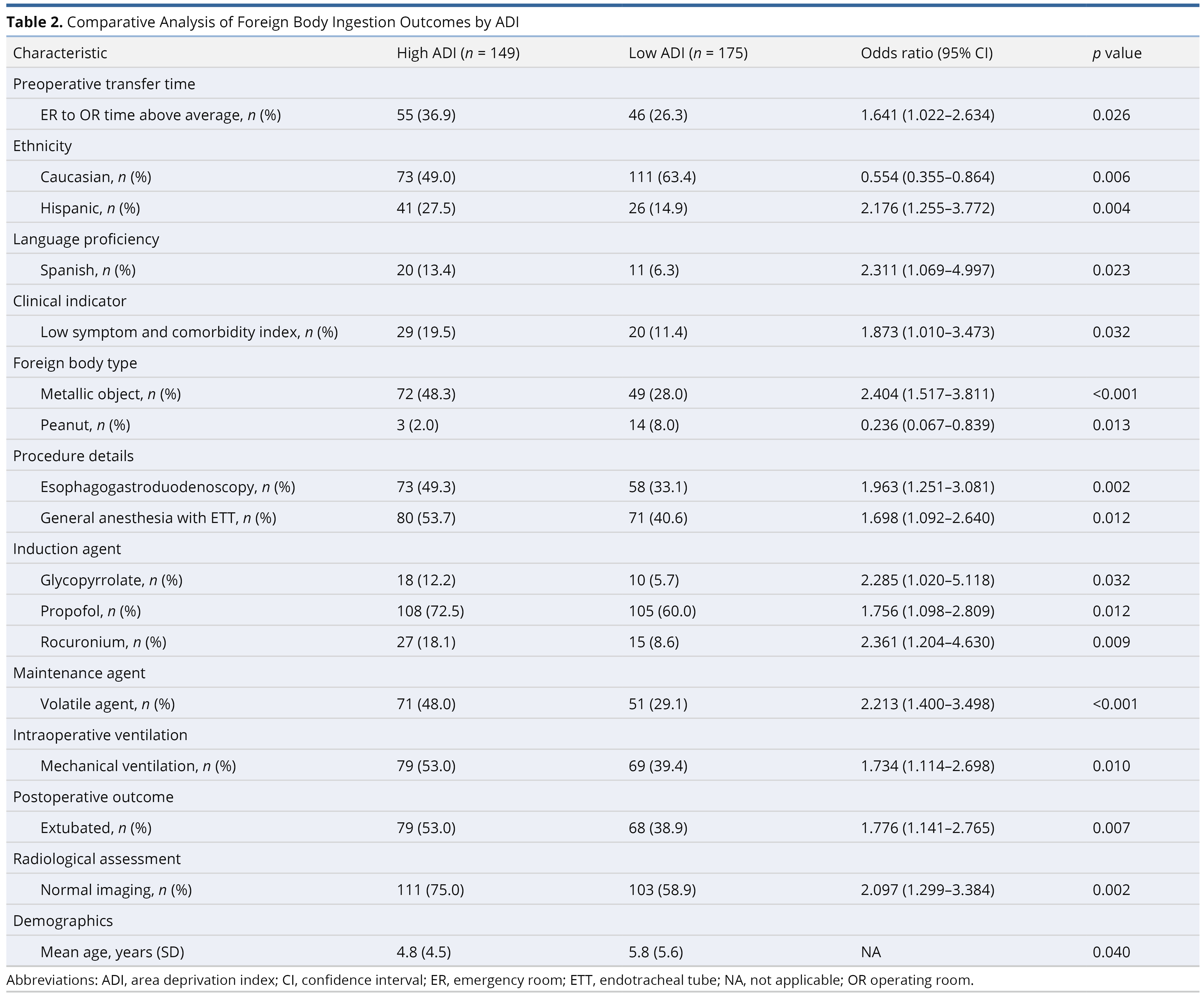
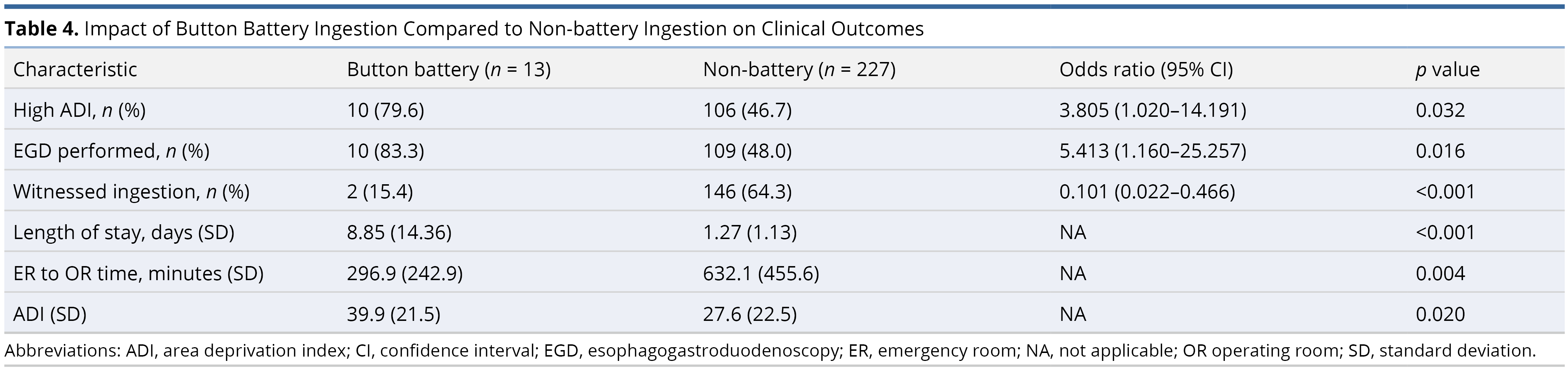
Results: Of the 324 patients with foreign body ingestion, 56.8% were Caucasian, 20.7% Hispanic, and 14.5% Black. The foreign bodies ingested included coins (33%), batteries (3.7%), and peanuts (5.3%). Foreign body locations were in the gastrointestinal tract (48.3%) and airway (14.2%). In the high ADI (> 50th percentile) cohort, patients were younger (p = 0.040) and more likely to be Spanish-speaking (95% confidence interval [CI] 1.069–4.997, p = 0.023). Button battery ingestion was associated with higher ADI (95% CI 1.020–14.191, p = 0.032) and a higher likelihood of endoscopy for esophageal foreign body ingestion (95% CI 1.160–25.257, p = 0.016). Illness severity was higher in patients with button battery ingestion (95% CI 1.646–36.606, p = 0.010).
Conclusion: Whether through increased education outreach at the pediatrician's office or the circulation of safety materials, communities with high ADI warrant our time and educational resources to reduce morbidity and mortality in their pediatric populations. Advocacy efforts among industry representatives, stakeholders, and policymakers will be paramount in eliminating button battery injuries.
Button battery ingestion presents a significant health risk, leading to morbidity and mortality in the pediatric population, especially in children younger than 5 years and with batteries larger than 2 cm in diameter. The rising incidence of button battery ingestion among children is likely attributable to their widespread use in consumer electronics. Mortality often results from esophageal mucosal, airway, or vascular injury [1,2]. Over the past two decades, there has been a sevenfold surge in the risk of complications associated with larger, more potent batteries. Reported incidences of ingestion range from 7 to 25% [3–5].
The Area Deprivation Index (ADI) measures socioeconomic deprivation in geographic areas, assessing social determinants of health such as healthcare access, disease severity, progression, and outcomes [6,7]. Studies have linked higher ADI with increased healthcare resource use, patient morbidity, and hospital costs [8,9]. Although previous research has highlighted the prevalence of accidental injuries in children from socioeconomically disadvantaged backgrounds [10], the specific impact of socioeconomic status on ingestion patterns remains inadequately explored. Significantly, a recent investigation conducted by Chen et al. has established a correlation between socioeconomic status and the ingestion of esophageal foreign bodies in pediatric patients [10]. These foreign bodies include a variety of items such as button batteries, magnets, sharp objects, and bones. However, the exact impact of socioeconomic factors on the ingestion patterns of specific button batteries has not been thoroughly investigated.
This study hypothesized that a lower socioeconomic status, as indicated by a higher ADI, was associated with an increased risk of button battery ingestion in children. It aimed to examine the complex relationship between socioeconomic disparities and pediatric health outcomes, focusing specifically on button battery ingestion incidents. By analyzing pediatric cases of button battery ingestion, this research sought to highlight the wider implications of socioeconomic factors on emergency healthcare access, treatment timelines, and overall patient recovery in acute pediatric injuries.
Patient Selection
We conducted a retrospective, single-center study involving 1,107 pediatric patients aged below 14 years, who were subjected to bronchoscopy or esophagoscopy for the removal of suspected aerodigestive foreign bodies at Maria Fareri Children’s Hospital, from January 1, 2010, to March 1, 2022. Older teenagers were not included in our study due to the institutional cutoff for pediatric surgical care being 14 years; consequently, individuals beyond this age are attended to by the adult services. Identification of subjects was achieved through the use of ICD-9 and ICD-10 codes pertaining to airway and esophageal foreign body ingestion. The study protocol received expedited approval from the Institutional Review Board (IRB #14834) at New York Medical College/Westchester Medical Center, adhering to the Health Insurance Portability and Accountability Act (HIPAA) guidelines. Inclusion criteria for our analysis were patients aged 14 years or younger from whom the aerodigestive foreign body was successfully extracted in the operating room utilizing bronchoscopy or esophagoscopy; all other individuals were excluded.
Data Collection
Patients included in the study underwent a thorough manual review of their medical records. Data collection encompassed demographic information, clinical and medical history, insurance status, time from the emergency room to the operating room, identity of foreign body, medical comorbidities, symptoms at presentation, radiologic imaging obtained, type of anesthesia, intraoperative ventilation, duration of anesthesia exposure, anesthesia induction and maintenance medications, postoperative disposition, complications, and length of hospital stay. Additionally, the residential addresses of the patients were employed to calculate an ADI.
Variable Definitions
The ADI was quantified on a scale from 0 to 100, where a value of 100 denoted the maximum level of socioeconomic deprivation. A high ADI was classified as exceeding the 50th percentile within our study cohort. The comorbidity index and symptom scale served as cumulative measures of individual comorbidities and presenting symptoms, respectively, with each being attributed a score of one. Consequently, a low score on either the comorbidity or symptom scale signified the absence of comorbidities or presenting symptoms. High illness severity was characterized by patients who necessitated continued intubation or admission to the Intensive Care Unit (ICU) following surgery. The metallic objects of interest in this study included both coins and button batteries.
Statistical Analysis
Descriptive statistics were utilized to present baseline characteristics. Normally distributed continuous variables were analyzed using the Student's t-test, while non-normally distributed continuous variables were compared using the Mann-Whitney U test. Categorical variables were compared between groups using the Chi-square test. Univariate binary regression was employed to identify statistically significant variables of interest. Subsequently, multivariate binary logistic regression was applied to evaluate independent predictors of high illness severity. A correlation matrix was examined to ascertain the presence of confounders. Analyses specific to foreign bodies were conducted within cohorts possessing all pertinent data. Statistical significance was determined at a threshold of p < 0.05. All analyses were performed utilizing SPSS (IBM SPSS Statistics for Windows, Version 29.0, Armonk, NY: IBM Corp).
Among 1,107 patients evaluated for aerodigestive foreign body ingestion, 324 were found to meet the inclusion criteria. Of these, 136 (42.0%) were female, with a median age of 3.1 years. The median ADI stood at 21.0, with an interquartile range of 10.0 to 38.0. The racial composition of the cohort included 184 (56.8%) Caucasian, 67 (20.7%) Hispanic, and 47 (14.5%) Black patients. The foreign bodies ingested included coins (33%), batteries (3.7%), and peanuts (5.3%). Foreign body locations were in the gastrointestinal tract (48.3%) and airway (14.2%). The most frequently observed presenting symptoms included cough (27.5%), vomiting (24.4%), and dysphagia (19.8%). Furthermore, asthma was documented as a comorbidity in 12.3% of the patients (Table 1).
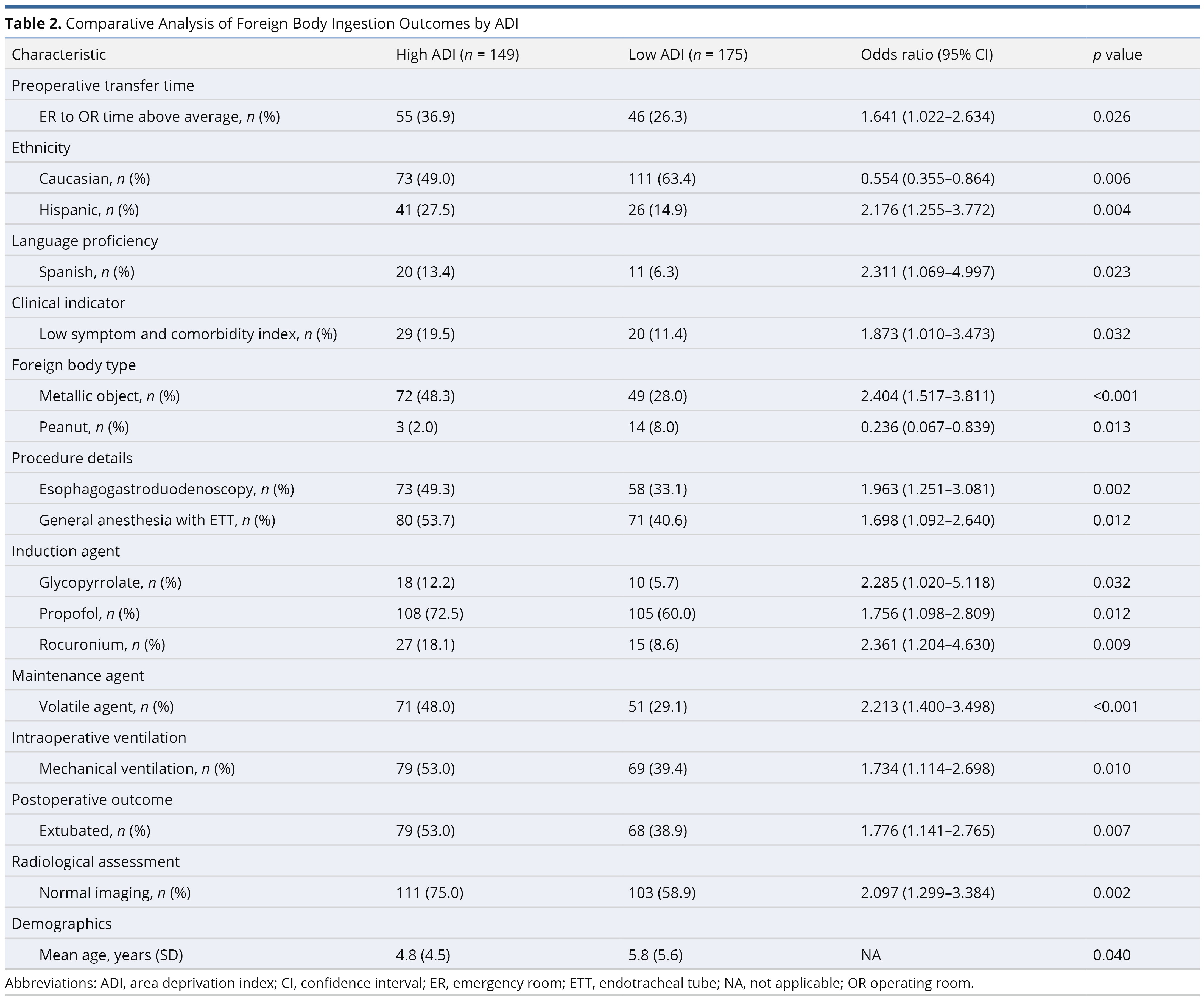
Patients with a high ADI were more likely to be Spanish-speaking (95% confidence interval [CI] 1.069–4.997, p = 0.023) and experienced longer wait times from the emergency room to the operating room (95% CI 1.022–2.634, p = 0.026) across all types of foreign body ingestions. Those in the high ADI group were also more inclined to have ingested metallic objects (95% CI 1.517–3.811, p < 0.001) and were more likely to undergo esophagogastroduodenoscopy (95% CI 1.251–3.081, p = 0.002). Normal imaging results were observed more frequently among high ADI patients (95% CI 1.299–3.384, p = 0.002). Additionally, the high ADI cohort tended to be younger (p = 0.040, Table 2).
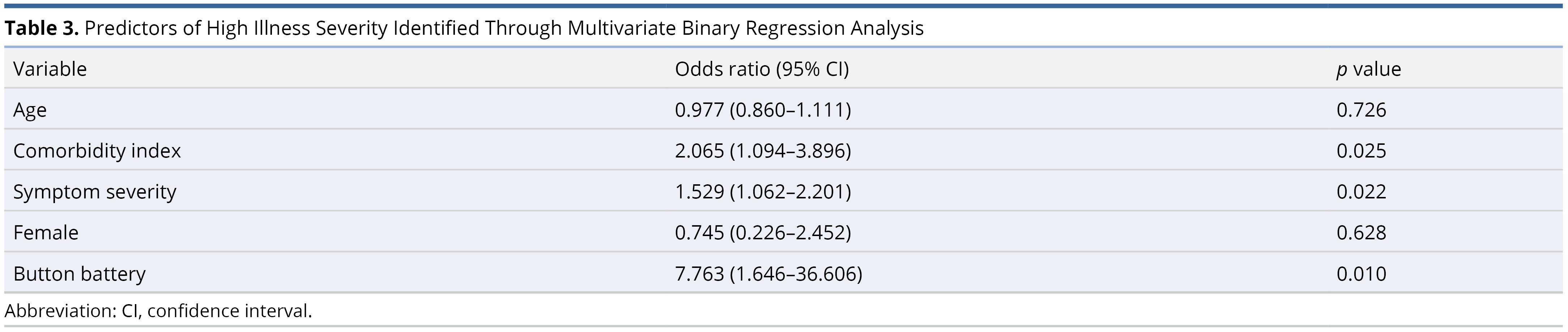
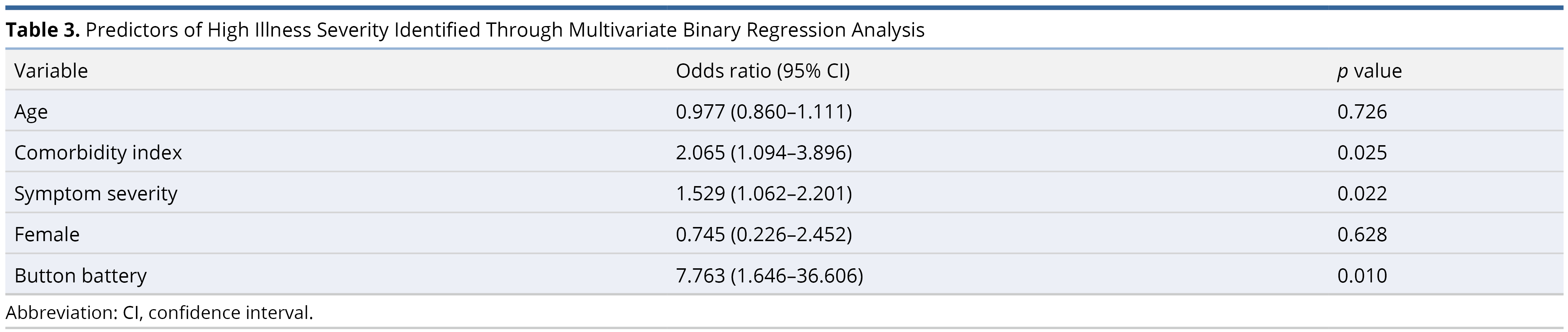
An escalation in illness severity following foreign body ingestion was associated with an increased number of comorbidities (95% CI 1.094–3.896, p = 0.025), a greater number of symptoms at presentation (95% CI 1.062–2.201, p = 0.022), and was particularly noted when the ingested foreign body was a button battery (95% CI 1.646–36.606, p = 0.010, Table 3).
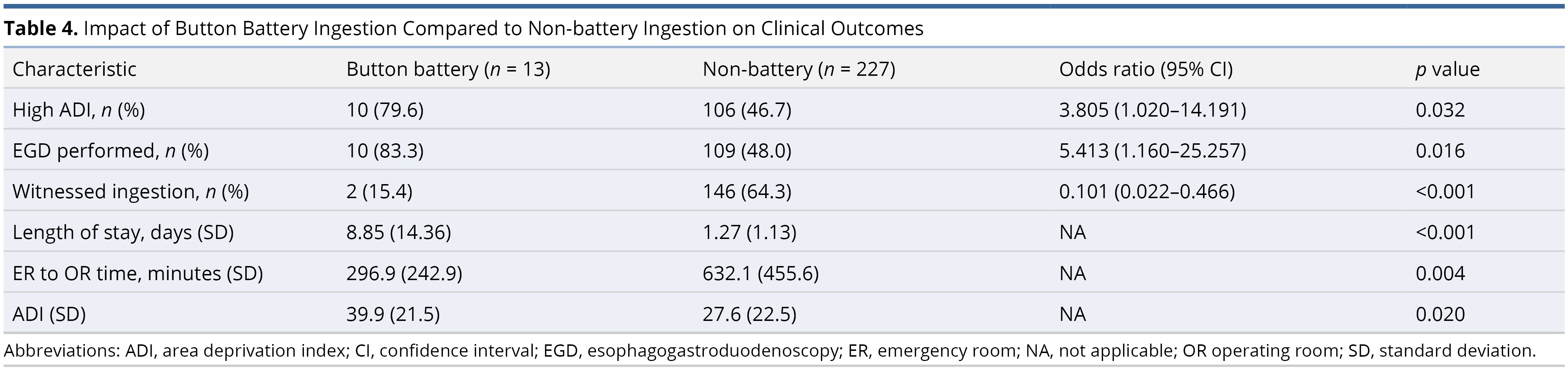
Button battery ingestion was associated with a higher ADI (95% CI 1.020–14.191, p = 0.032) and an elevated need for esophagogastroduodenoscopy (95% CI 1.160–25.257, p = 0.016). Patients with button battery ingestion were less likely to have the ingestion event witnessed (95% CI 0.022–0.466, p < 0.001). Notably, there was a reduction in the time from the emergency room to the operating room (p = 0.004) and an increase in the length of hospital stay (p < 0.001) following button battery ingestion. An elevated ADI was observed in patients who ingested button batteries (p = 0.020, Table 4).
ADI Influences on Button Battery Ingestion Risks
Our research identified a significant correlation between the ADI and the incidence of metallic object ingestions, specifically button batteries. We found that patients from higher ADI settings were more prone to being uninsured, experiencing unwitnessed button battery ingestions, and sustaining severe injuries. These findings imply that socioeconomic disparities markedly affect both the risk and severity of button battery ingestions.
We hypothesized that families from economically disadvantaged communities might postpone seeking medical care for their children due to various obstacles [11]. Additionally, the absence of consistent, personalized childcare in these communities could lead to a greater frequency of unwitnessed ingestions, given that families in higher ADI settings may lack dependable access to quality childcare, thereby heightening the risk of button battery ingestion.
Corroborating our findings, Chen et al. underscored housing instability, material deprivation, and elevated poverty levels as significant predictors of increased risks for ingesting hazardous foreign bodies, including button batteries [10]. Ijaduola et al. reported a higher incidence of ear, nose, and throat foreign bodies among Nigerian children from lower socioeconomic backgrounds [12], while Hur et al. established a correlation between lower income, public insurance, and the occurrence of retained esophageal foreign bodies in Los Angeles [13]. Additionally, research by Sinclair et al. in Atlanta, Georgia, showed a disproportionate incidence of esophageal button battery ingestions among Black children, with the need for interpreter services suggesting extended button battery impaction durations [14].
Impact of Delayed Medical Intervention
Delayed diagnosis and medical intervention significantly contribute to the increased morbidity and mortality associated with button battery ingestion. Children who present with aerodigestive symptoms following possible button battery ingestion necessitate a high degree of clinical suspicion to facilitate prompt battery removal. Unfortunately, this urgency is often compromised in communities with a higher ADI, where limitations in healthcare knowledge or unobserved ingestion incidents may occur [15].
The difficulty in diagnosing button battery ingestion is further exacerbated by the nonspecific and variable symptoms children may exhibit. While some children may show no symptoms, others can exhibit a wide range of symptoms including fever, vomiting, lethargy, reduced appetite, irritability, stridor, wheezing, cough, and hemoptysis [16]. A review of national button battery data from 2010 revealed that 27% of major adverse outcomes and 54% of fatalities were due to misdiagnosis, a consequence of the nonspecific symptomatology. The failure to promptly recognize and manage button battery ingestion can lead to life-threatening conditions such as aortoesophageal fistulas and severe exsanguination [1].
In our study cohort, the patient with the highest ADI developed a tracheoesophageal fistula after a delay exceeding 12 hours in button battery removal, ultimately leading to the patient's death. The occurrence of tracheoesophageal fistula in button battery ingestion cases ranges from 2% to 8%, with mortality rates between 2% and 17%, underscoring the critical importance of timely medical intervention [17–20].
Diverse Mechanisms of Button Battery Harm
The mechanisms of injury following button battery ingestion are multifaceted, involving local pressure necrosis, metallic toxicity, corrosion from the battery's contents, and electrical injury [21]. The employment of high-voltage lithium cells, capable of generating hydroxide radicals, significantly increases the risk of vascular injuries, esophageal burns, stenosis, fistulization, and even vocal cord paralysis. These complications can manifest as rapidly as two hours following the lodgment of the button battery [1,22,23].
A comprehensive review by Varga et al. in 2018, analyzing data from 136,191 patients, reported the mortality risk associated with button battery ingestion as notably low, at 0.04% [21]. However, the primary causes of death in these cases were identified as massive hemorrhage due to the formation of a great vessel fistula or asphyxiation, which resulted from either blood aspiration or bronchopneumonia [21]. These outcomes underscore the grave consequences of button battery ingestion, highlighting the urgency of addressing these injuries.
The physical location and orientation of the ingested button battery within the esophagus are critical in determining the nature and severity of subsequent complications. Impaction against the anterior esophageal wall can cause injuries to the trachea, vascular system, or vocal cords, potentially leading to the development of tracheoesophageal fistulas. On the other hand, a button battery that becomes lodged with its orientation towards the posterior esophageal wall is more likely to be associated with spondylodiscitis [24].
Moreover, long-term or late-stage complications, such as the development of esophageal strictures or recurrent laryngeal nerve injuries, are also significant concerns. These issues may not manifest until weeks to months following the initial ingestion of the button battery, indicating the prolonged risk and the need for extended monitoring of affected individuals [1].
Additionally, long-term or late-stage complications, including the development of esophageal strictures or recurrent laryngeal nerve injuries, present significant concerns. These complications may not become apparent until weeks or months after the initial ingestion of the button battery, highlighting the extended risk and underscoring the necessity for prolonged monitoring of affected individuals [1].
Predictors of Button Battery Ingestion Outcomes
The literature presents a vital algorithm for predicting outcomes in button battery ingestion incidents. Scalise et al. developed a multivariate prediction model to identify key predictors of severe outcomes, including the detection of an esophageal button battery on initial imaging, symptomatic presentation, and a button battery size greater than or equal to 2 cm [25]. Eliason et al. also underlined the critical importance of the duration of impaction, anode orientation of the battery, its voltage, and metallic composition as key predictors of chronic complications, highlighting the need for extended monitoring [26].
Intervention Strategies to Mitigate Injury
To mitigate the severity of injuries resulting from button battery ingestion, prompt intervention strategies are essential. The effectiveness of honey or sucralfate in neutralizing tissue pH and reducing mucosal damage has been demonstrated, especially when administered within five minutes of ingestion [27]. Moreover, irrigation with 0.25% acetic acid after battery removal has proven effective in preventing delayed mucosal injuries, perforations, and the formation of strictures [28].
Standardizing Management of Button Battery Ingestion
Initiatives to unify the approach to button battery ingestion have been led by the Endoscopy Committee of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN), which recommends the urgent endoscopic removal of an impacted button battery within two hours [29]. Nevertheless, the application of these consensus guidelines in patient care remains inconsistent, affected by institutional experience and the availability of specialized resources. High-risk individuals, specifically those aged under 5 years or with button batteries larger than 2 cm in diameter, are prioritized for endoscopic intervention to prevent possible complications [26,29].
Expedited Response to Button Battery Ingestions
Our research indicated that patients with a higher ADI typically encounter prolonged times from the emergency room to the operating room when presenting with aerodigestive foreign bodies. This pattern highlights the role of socioeconomic factors in the accessibility and promptness of healthcare services. Conversely, in cases of button battery ingestions, our pediatric trauma center has introduced an expedited emergency activation protocol. This measure has effectively shortened the wait times from the emergency room to the operating room, proving that clinical urgency can surmount socioeconomic differences to guarantee timely care. The protocol is applied irrespective of the patient's socioeconomic status, reinforcing a commitment to equitable healthcare provision centered on clinical requirements.
Streamlining Hospital Care Pathways
Several variables contribute to the prolonged intervals from the emergency room to the operating room for patients without button battery ingestions. These variables encompass hospital practices, the patient's clinical condition upon arrival, the preparedness of surgical and anesthesia teams, operating room scheduling, and administrative procedures. Together, they underscore the complexities inherent in healthcare logistics and the potential for inefficiencies within patient care pathways.
To address these challenges, a concerted effort is essential to streamline hospital processes. Optimizing each step from emergency room admission to operating room treatment, especially for high-risk patients such as those with button battery ingestions, is crucial. Such optimization can significantly enhance patient outcomes. This approach not only improves the efficiency of healthcare delivery but also highlights the critical importance of swift intervention in emergency situations.
Optimizing Esophageal Battery Removal Protocols
Our institutional policy mandates the immediate endoscopic removal of esophageal button batteries, in adherence to the NASPGHAN guidelines. In instances of severe mucosal damage or when retrieval is delayed beyond 12 hours, computed tomography scans are utilized, consistent with the guidelines of the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) [22]. Revisions to our guidelines in 2016 elevated the priority of esophageal button battery removal to an emergent procedure, thereby streamlining the process for booking operating rooms to reduce wait times affected by operational and staff availability. Furthermore, esophagrams are performed to verify the absence of additional injuries prior to dietary progression. In high-risk situations, specifically involving patients under the age of 5 years or where the button battery size exceeds 2 cm, endoscopic interventions are initiated within 48 hours [25].
Risk Stratification and Management Optimization
Scalise et al.'s study emphasizes the critical need for evidence-based risk stratification in instances of button battery ingestion. It recommends prioritizing the transfer of symptomatic patients, particularly those with large esophageal batteries, to tertiary children's hospitals outfitted with extensive endoscopic and surgical facilities [25]. This protocol assumes critical importance for individuals residing in underserved regions characterized by a high ADI, identified as possessing a heightened risk for button battery ingestion. Our strategy prioritizes early intervention, encompassing parental education, minimizing battery exposure, and conducting thorough initial assessments to mitigate the risk of injury from button battery ingestion. A multidisciplinary approach, orchestrated by the button battery task force and endorsed by the American Academy of Pediatrics, underpins the timely and efficient management of these cases [30–32].
Innovative Solutions for Button Battery Safety
The innovation of a deactivation technique for coin cell batteries by Landsdowne Labs® marks a substantial progression in mitigating mucosal injuries resulting from button battery ingestion [33]. Furthermore, to elevate global consciousness and disseminate essential information concerning aerodigestive foreign body ingestions, the introduction of the Global Injury Research Collaborative application (GIRC app)® has been undertaken. This smartphone application functions as an anonymized international database for healthcare professionals, cataloging diverse facets of foreign body ingestion incidents [34].
Limitations
This single-center, retrospective study encounters limitations stemming from potential inconsistencies in documenting variables, variations in care, and the urgency levels assigned to operating room triage for button battery extractions prior to 2016, coupled with the descriptive nature of our data. Our chart review faced obstacles in gathering data on the degree of mucosal injury, long-term outcomes, and chronic complications, attributable to variability in the documentation of patient charts. Furthermore, the transfer of a subset of patients to our institution after their initial diagnosis introduces a potential selection bias. More complex cases may have been preferentially directed to our Level 1 trauma center, potentially resulting in care delays. The risk factors for button battery ingestion among children from various socioeconomic backgrounds are expected to be complex, involving an intricate mix of wider social and familial factors. This study was unable to analyze factors that might contribute to this risk, such as the number of children or siblings in a household and periods of unsupervised play, due to the constraints of our chart review methodology.
This study emphasizes the increased incidence of button battery ingestion within families residing in areas with a higher ADI, revealing a significant disparity in pediatric healthcare. It underscores the importance of enhanced parental education through strategies such as initiatives in pediatric offices or the dissemination of safety materials, especially in communities with high ADI. These efforts are vital to decreasing morbidity and mortality rates among children. Crucially, collaboration with industry representatives, stakeholders, and policymakers is essential to eliminate button battery-related injuries on a global scale. Establishing a national registry or conducting a multicenter study would offer a broader perspective on the healthcare inequalities related to aerodigestive foreign body ingestions across the United States.
Received date: January 16, 2024
Accepted date: February 27, 2024
Published date: April 02, 2024
The manuscript has not been presented or discussed at any scientific meetings, conferences, or seminars related to the topic of the research.
The study adheres to the ethical principles outlined in the 1964 Helsinki Declaration and its subsequent revisions, or other equivalent ethical standards that may be applicable. These ethical standards govern the use of human subjects in research and ensure that the study is conducted in an ethical and responsible manner. The researchers have taken extensive care to ensure that the study complies with all ethical standards and guidelines to protect the well-being and privacy of the participants.
The author(s) of this research wish to declare that the study was conducted without the support of any specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The author(s) conducted the study solely with their own resources, without any external financial assistance. The lack of financial support from external sources does not in any way impact the integrity or quality of the research presented in this article. The author(s) have ensured that the study was conducted according to the highest ethical and scientific standards.
In accordance with the ethical standards set forth by the SciTeMed publishing group for the publication of high-quality scientific research, the author(s) of this article declare that there are no financial or other conflicts of interest that could potentially impact the integrity of the research presented. Additionally, the author(s) affirm that this work is solely the intellectual property of the author(s), and no other individuals or entities have substantially contributed to its content or findings.
It is imperative to acknowledge that the opinions and statements articulated in this article are the exclusive responsibility of the author(s), and do not necessarily reflect the views or opinions of their affiliated institutions, the publishing house, editors, or other reviewers. Furthermore, the publisher does not endorse or guarantee the accuracy of any statements made by the manufacturer(s) or author(s). These disclaimers emphasize the importance of respecting the author(s)' autonomy and the ability to express their own opinions regarding the subject matter, as well as those readers should exercise their own discretion in understanding the information provided. The position of the author(s) as well as their level of expertise in the subject area must be discerned, while also exercising critical thinking skills to arrive at an independent conclusion. As such, it is essential to approach the information in this article with an open mind and a discerning outlook.
© 2024 The Author(s). The article presented here is openly accessible under the terms of the Creative Commons Attribution 4.0 International License (CC-BY). This license grants the right for the material to be used, distributed, and reproduced in any way by anyone, provided that the original author(s), copyright holder(s), and the journal of publication are properly credited and cited as the source of the material. We follow accepted academic practices to ensure that proper credit is given to the original author(s) and the copyright holder(s), and that the original publication in this journal is cited accurately. Any use, distribution, or reproduction of the material must be consistent with the terms and conditions of the CC-BY license, and must not be compiled, distributed, or reproduced in a manner that is inconsistent with these terms and conditions. We encourage the use and dissemination of this material in a manner that respects and acknowledges the intellectual property rights of the original author(s) and copyright holder(s), and the importance of proper citation and attribution in academic publishing.
This study reframes postoperative opioid stewardship by showing that prescribing is not a uniform clinical reflex to pain. Instead, it is a multifactorial behavior shaped by procedure type, surgeon experience, and patient characteristics. An analysis of more than two thousand ambulatory otolaryngology cases revealed that surgical procedure exerts the strongest influence, with oropharyngeal operations linked to nearly threefold higher opioid quantities than nasal surgeries. Younger, recently trained surgeons prescribed substantially less. Counterintuitive racial and comorbidity patterns further exposed how implicit bias and clinical caution may coexist in prescribing behavior. By disentangling these procedural, provider, and patient determinants, the study challenges one-size-fits-all mandates and calls for precision prescribing frameworks that balance effective analgesia with the reduction of opioid-related harm. This paradigm shift urges clinicians and policymakers to replace volume-based control with individualized, evidence-driven stewardship grounded in real surgical practice.
This article explores the risk posed by button battery (BB) ingestion in children. The study correlates higher Area Deprivation Index (ADI) levels with increased BB ingestion incidents, suggesting socioeconomic factors play a crucial role. Methodologically, the retrospective analysis of pediatric patients who underwent bronchoscopy or esophagoscopy for suspected aerodigestive foreign body (FB) ingestion offers comprehensive insights. However, the article, while enlightening, reveals critical concerns such as potential procedural inconsistencies, limited by its single-center, retrospective nature, and a lack of clarity in defining severity in its data collection. These issues, alongside the absence of comprehensive statistical information like 95% confidence intervals, raise questions about the study's rigor. Consequently, in its present form, the article falls short of the standards required for publication, necessitating revisions for enhanced clarity and methodological robustness.
The article explores the relationship between Area Deprivation Index (ADI) levels and button battery (BB) ingestion in pediatric populations, highlighting a crucial aspect of pediatric care. It underscores the heightened risk in communities with higher ADI, emphasizing the need for targeted educational and preventive measures. However, the manuscript has limitations. It lacks clear research hypotheses in the introduction, creating ambiguity about the study's purpose. The presentation of findings in Tables 2-4 relies solely on p-values without accompanying 95% confidence intervals (CIs), which are crucial for understanding effect size and precision. Combining p-values and CIs is recommended for comprehensive interpretation. Additionally, displaying odds ratios (ORs) with 95% CIs in a separate column would enhance clarity. The authors should improve their statistical reporting for better transparency and completeness in research publications. Although the study establishes a notable socioeconomic connection to BB ingestion, these concerns indicate that it necessitates further revision before it can be deemed publication ready.
While current studies emphasize the heightened risk of accidental injuries among socioeconomically disadvantaged children, the specific impact of socioeconomic status on pediatric button battery ingestion remains largely unexplored. An exhaustive search on PubMed identifies only one study (Chen T et al. Pediatric Esophageal Foreign Bodies: The Role of Socioeconomic Status in Ingestion Patterns. Laryngoscope. Online ahead of print), published in January 2024, that directly tackles this issue. The current research, in conjunction with previous findings, highlights the significant influence of socioeconomic factors on the consequences of button battery ingestions, urging the need for specialized public health strategies and educational efforts to address these inequalities. Utilizing diverse methodologies, regional analyses, and socioeconomic indicators, this study provides comprehensive insights into the influence of social health determinants on pediatric emergencies, particularly those involving button battery ingestion. This research emphasizes the critical need for its publication following minor revisions, showcasing the importance of understanding the multifaceted impact of socioeconomic status on health outcomes in emergency pediatric care.
The article under review significantly advances pediatric healthcare research by examining the link between Area Deprivation Index (ADI) and the risk of button battery ingestion in children. Its publication is justified by the vital insights it provides into the complex relationship between socioeconomic status and health outcomes, especially within pediatric emergency care. The study underscores the importance of incorporating socioeconomic factors into healthcare delivery and emergency protocols, highlighted by its findings on the potential for increased ER to OR waiting times for patients with higher ADI and the consequential effects on patient outcomes. Furthermore, the study's emphasis on a thorough examination of factors affecting ER to OR times, such as hospital protocols and the urgency of patient conditions, is crucial for enhancing management approaches and patient care results. The call for clarity in distinguishing between 'metallic object' and 'button battery' ingestions underscores the importance of precision in research, elevating the study's applicability to clinical practice. This research is likely to engage readers from the medical, public health, and policy-making sectors, encouraging discussions aimed at improving healthcare access and interventions for at-risk pediatric groups. With minor revisions needed, this article is nearly ready for publication.
Khan A, Zhang A, Moscatello A, et al. High area deprivation index is associated with an increased risk of button battery ingestion in a pediatric cohort. Arch Otorhinolaryngol Head Neck Surg 2024;8(1):3. https://doi.org/10.24983/scitemed.aohns.2024.00182