2017/04/09
Sudden deafness is an otologic emergency that occurs over a period of less than 3 days. This is particularly disconcerting for professionals like professional drivers and musicians as their dependence on their hearing levels is critically important.
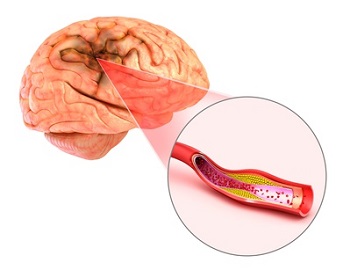
The medical fraternity has now concluded that the cause of sudden deafness is identifiable in only 10% of the cases. One of the commonest causes is stroke, which makes it all the more important. The logic being that one third of stroke survivors are dependent on others one year after the attack and rehabilitation depends on effective communication between the patient and the doctor. Post-stroke sudden deafness can hinder communication between patients and healthcare professionals, thereby restricting participation in rehabilitation programs and limiting improvements in physical performance. However, the relationship between stroke and subsequent sudden deafness remains unclear.
Recently, an observational study was conducted by Kuo et al. to investigate the relationship between stroke and sudden deafness wherein the nationwide Longitudinal Health Insurance database was used for selecting the study (stroke) and comparison (non-stroke) groups. The database was sourced from Taiwan National Health Insurance, which is responsible for 99% of the healthcare costs in Taiwan. The study and comparison groups were identified to study the correlation between stroke and subsequent development of sudden deafness. Both of the groups were followed over a period of five years.
The study group was identified based on specific criteria (i.e. those diagnosed with stroke by qualified health professionals; and those with one or more “in patient” visits to the hospital, or two or more ambulatory visits). Subjects who were less than 18 years of age were excluded from the group. The number of patients in the study group was 11,115. For the comparison group, three patients were randomly matched to each patient in the study group where age sex and year of diagnosis were the same. However subjects in the comparison group were healthy and had not suffered from stroke. The number of patients in the comparison group was 33,345 hence maintaining the ratio of one study patient compared to three patients from the comparison group.
The results were analyzed based on the following:
The implications are grave considering that if there is a hearing impairment and it is missed out; this could adversely affect the clinical outcome as the rehabilitation program may not be very effective due to lack of comprehension. Concurrently, the patient may begin to withdraw socially due to a hearing impairment and this could slow down the recovery and improvement process significantly. Close monitoring of hearing status among stroke patients may facilitate early detection and timely management of comorbid hearing deficits through the fitting of hearing aids. Enhancing one’s ability to communicate can help to relieve their psychological burden and facilitate rehabilitation.
The major advantage and strength of this study is that the sample size is very large; hence the selection bias is very low. Conversely as this is a National Healthcare Program, which oversees the reimbursement of healthcare costs for up to 99% of the 23.5 million residents of Taiwan, following up of study and comparison groups is easy and there are nearly no fallouts. Concurrently as the co-payment or payout that the consumer has to make is very low (3-15 US dollars), utilization of medical services is very high. Hence the probability of under reporting is highly improbable.
The major disadvantage of the study is that the severity of stroke is not captured thus limiting the accuracy of the study. The logic being that it is possible that the severity of stroke may have a correlation with the probability of getting sudden deafness. In addition, it is more than evident that the number of stroke patients who contract sudden deafness could well be much higher than reported. The logic being that stroke patients who were bed ridden or were suffering from cognitive impairment may have been missed out from the diagnosis of sudden deafness due to the challenge in diagnosis.
The study has identified a strong link between stroke and subsequent sudden deafness. Thus early hearing loss in stroke patients is a distinct possibility and clinicians should monitor hearing acumen closely so as to ensure that the diagnosis is not missed out. To reiterate a case in point, the first year immediately after an attack of stroke is particularly important considering that this is the period when the risk of sudden deafness increases more than fivefold as compared to those not suffering from stroke.
Kuo C.L., Shiao A.S., Wang S.J., Chang W. P., Lin Y.Y. Risk of sudden sensorineural hearing loss in stroke patients. A 5-year nationwide investigation of 44,460 patients. Medicine (2016) 95:36 (e4841).